Table of Contents
Introduction
When your dog suddenly collapses, stiffens, or convulses, it’s terrifying. Many pet owners aren’t prepared for that first seizure, and even fewer realize it could mark the start of a lifelong condition. Canine epilepsy isn’t rare, but it’s often misunderstood. One moment, your dog is chasing a ball; the next, they’re disoriented, trembling, or unconscious. It’s a helpless feeling.
I’ve seen firsthand how devastating seizures can be for both dogs and their families. But I’ve also seen many of those same dogs live full, happy lives with the right treatment and guidance.
This article unpacks seven must-know facts about canine epilepsy, from common seizure triggers and medications to long-term prognosis and daily management. Grounded in the latest veterinary research, it’s written to help you recognize, respond to, and manage canine epilepsy with confidence.
There’s more hope and science than most people realize.
Medical Disclaimer:
This article is for informational purposes only and does not constitute veterinary advice. Always consult your veterinarian or a board-certified veterinary neurologist before starting or changing your pet’s treatment plan for canine epilepsy.
✅ Key Takeaways
- Canine epilepsy affects up to 5.7% of dogs and typically begins between 6 months and 6 years of age.
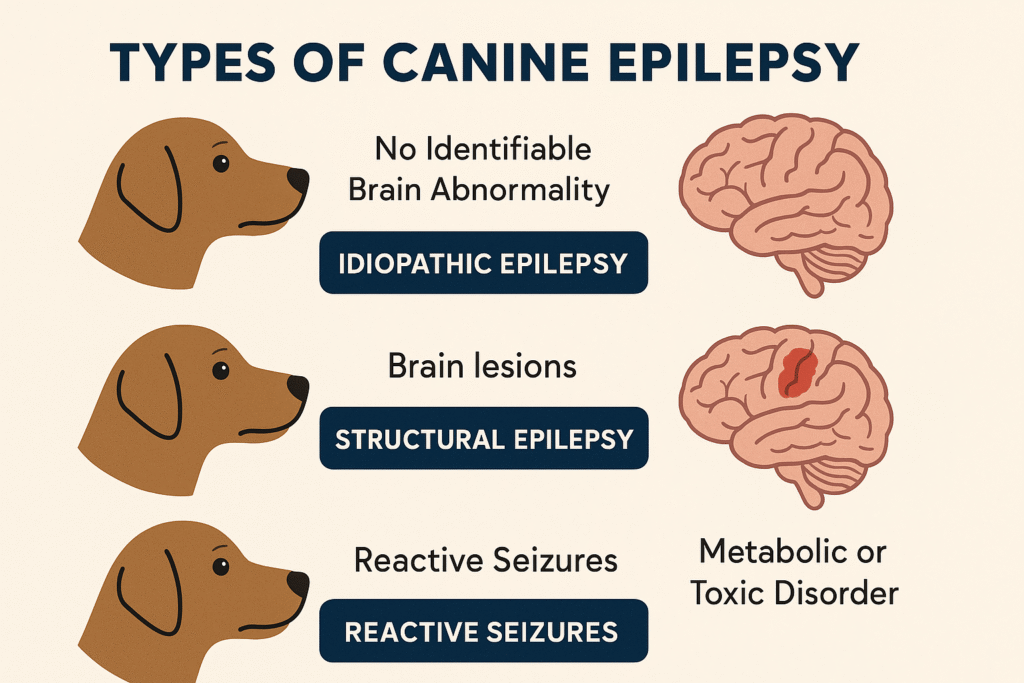
- There are three main types: idiopathic (genetic), structural (brain-related), and reactive (metabolic/toxic).
- Seizure triggers like stress, heat, or disrupted routines can worsen episodes but are often manageable.
- Diagnosis is based on history, ruling out other conditions, and sometimes advanced imaging.
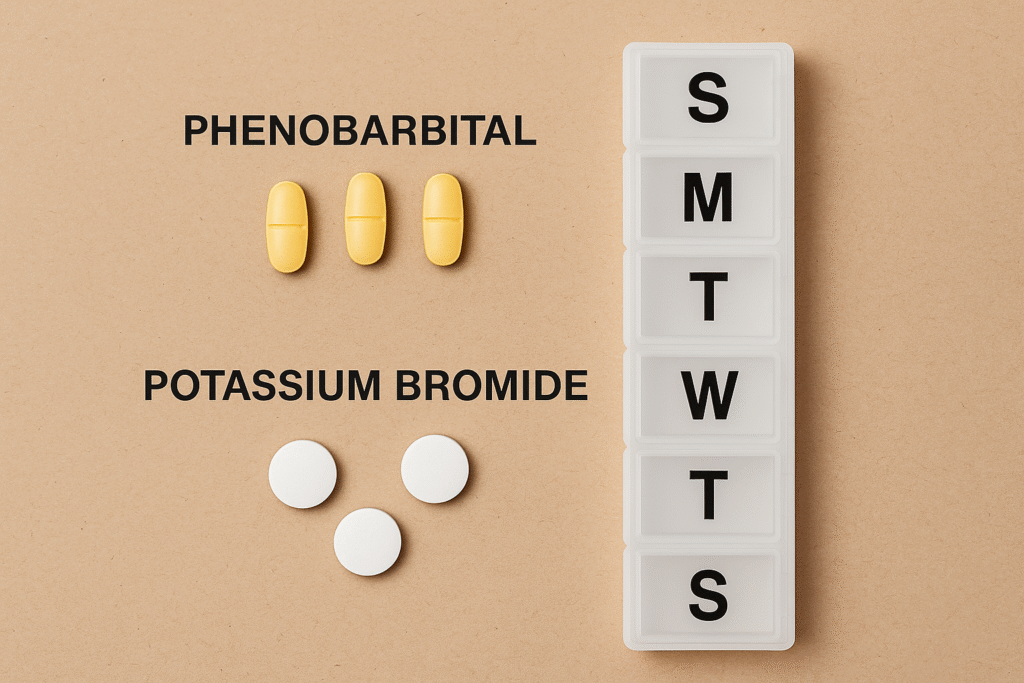
- Common medications include phenobarbital, potassium bromide, imepitoin, and levetiracetam, each with benefits and side effects.
- Around 30% of dogs have canine epilepsy that is resistant to medication alone; polytherapy may help.
- Many dogs can live normal lives if their seizures are well-managed and their quality of life is supported.
This guide includes everything you need to understand your dog’s condition better and help them thrive.
1. Understanding Canine Epilepsy
You can also visit: https://doglifeexpert.com/cushings-disease-in-dogs-2025/
Canine epilepsy is a chronic brain disorder marked by recurrent, unprovoked seizures. These seizures occur when abnormal electrical activity in the brain disrupts normal function, causing anything from mild twitching or staring spells to full-body convulsions. Epilepsy is considered “idiopathic” when no structural brain disease or metabolic cause can be found.
It’s the most common long-term neurological condition in dogs, with an estimated prevalence of 0.5% to 5.7% of the canine population, according to a study by Berendt et al.. Certain breeds like Border Collies, Australian Shepherds, and Beagles are genetically predisposed, and seizures often begin between 6 months and 6 years of age.
While watching a seizure can be terrifying, not every episode is life-threatening. With a proper diagnosis, individualized treatment, and consistent management, many dogs with canine epilepsy go on to live active, fulfilling lives.
Types of Canine Epilepsy
There are three primary forms:
- Idiopathic Epilepsy (IE): Most common. No visible brain abnormality. Often genetic in origin.
- Structural Epilepsy: Caused by an identifiable brain issue such as a tumour, stroke, or trauma.
- Reactive Seizures: Result from temporary problems outside the brain, like liver disease or poisoning.
Idiopathic epilepsy typically develops in dogs aged 6 months to 6 years. Some breeds, including Border Collies and Beagles, are more genetically predisposed, as noted by Mickelson & Steinberg.
Understanding the type of epilepsy your dog has helps guide both prognosis and treatment options.
2. Identifying Triggers in Dogs with Canine Epilepsy

One of the most overlooked parts of managing canine epilepsy is recognizing what sets seizures off. While some seizures appear out of the blue, many have subtle or recurring triggers. Identifying and avoiding these can significantly reduce seizure frequency.
A study in The Veterinary Record found that over 60% of owners were able to pinpoint consistent triggers after keeping a detailed log (De Risio et al.). These commonly include:
- Stressful events (vet visits, grooming, fireworks)
- Changes in routine or sleep patterns
- Heat or vigorous exercise
- Excitement or overstimulation
- Hormonal cycles (in intact females)
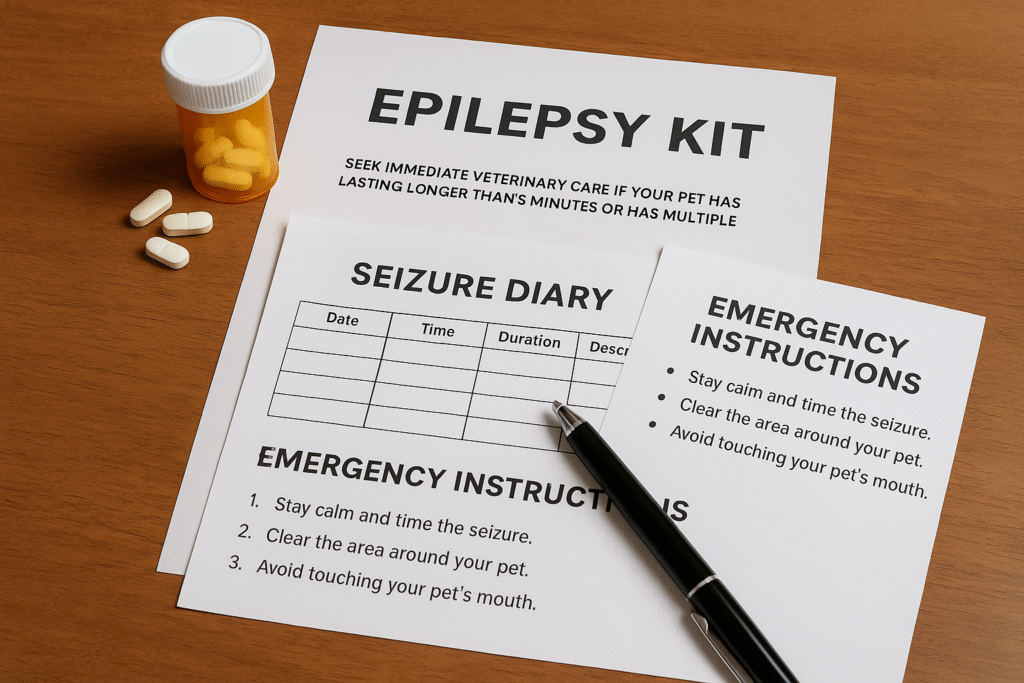
Your Action Plan: Create a Seizure Diary
Record when seizures happen, what your dog was doing beforehand, environmental conditions, and any recent changes in diet or medication. This helps reveal patterns that you might otherwise miss and provides your vet with valuable data to adjust treatment.
If you’re consistent, tracking may help reduce your dog’s seizures dramatically.
3. Diagnosing Canine Epilepsy with Veterinary Expertise

Getting a diagnosis of canine epilepsy isn’t as straightforward as running a single test. Because there’s no specific “epilepsy test,” veterinarians must rule out other possible causes through a structured process of elimination.
The Diagnostic Process for Canine Epilepsy: What to Expect
Diagnosing canine epilepsy isn’t about a single test; it’s a step-by-step process your veterinarian follows to rule out other causes of seizures and confirm epilepsy. Here’s what’s typically involved:
1. Thorough Clinical History
Your vet will begin by asking about:
- The first seizure event: what it looked like, how long it lasted, and how your dog behaved afterward.
- Any patterns or triggers: This is where a seizure diary becomes invaluable. Record things like diet, stress levels, time of day, and recent activities before each episode.
- Your dog’s age, breed, and health history can point toward breed-specific risks or inherited forms of idiopathic epilepsy.
2. Physical and Neurological Examination
A complete physical and neurological exam helps rule out signs of other conditions that can mimic seizures, such as fainting (syncope), vestibular disease, or pain-related tremors. Your vet will check reflexes, gait, pupil responses, and head posture for clues about possible structural brain involvement.
3. Routine Bloodwork and Bile Acid Tests
These tests evaluate for metabolic causes of seizures, including:
- Hypoglycemia (low blood sugar)
- Hepatic encephalopathy (from liver dysfunction)
- Electrolyte imbalances
- Toxins or infections
Bile acids testing helps assess liver function, particularly in breeds prone to portosystemic shunts (like Yorkshire Terriers).
4. Advanced Imaging: MRI or CT Scan
When your veterinarian suspects structural epilepsy meaning the seizures may be caused by a physical problem in the brain they’ll often recommend advanced imaging. This is especially important if your dog’s seizures begin very early (before 6 months of age) or later in life (after 6 years), or if there are abnormal findings on the neurological exam.
What Do MRI and CT Scans Show?
Both imaging tools allow vets to “look inside” your dog’s brain to identify or rule out physical causes of seizures, such as:
- Brain tumours – These can press on brain tissue, triggering seizures.
- Strokes or hemorrhage – Interruption of blood flow or bleeding in the brain.
- Congenital abnormalities – Malformations present from birth, like hydrocephalus.
- Inflammation or infection – Meningitis, encephalitis, or protozoal infections can irritate the brain and cause seizures.
MRI vs. CT: What’s the Difference?
- MRI (Magnetic Resonance Imaging):
Provides highly detailed images of soft tissue structures in the brain. It’s the gold standard for diagnosing subtle or complex causes of canine epilepsy. Most dogs will need general anesthesia to keep them still during the scan. - CT (Computed Tomography):
Offers good visualization of bone and brain tissue but is less sensitive than MRI for soft tissues. It’s quicker and sometimes more available, particularly in smaller clinics.
In either case, imaging is often paired with cerebrospinal fluid (CSF) analysis to detect signs of infection or inflammation that might not show up on scans alone.
These advanced tools give your veterinary team the best possible insight into why your dog is having seizures—and how to treat them most effectively.
5. Cerebrospinal Fluid (CSF) Analysis
In select cases, a spinal tap is done to examine the cerebrospinal fluid surrounding the brain and spinal cord. This can detect:
- Inflammation or infection (e.g., meningitis, encephalitis)
- Elevated protein levels (a sign of certain brain diseases)
- Cancer cells, in rare cases of CNS lymphoma
CSF analysis is often performed alongside MRI for a more complete picture of brain health.
A dog is usually diagnosed with idiopathic epilepsy if they have repeated seizures over 24 hours apart, normal physical and neurological exams, and no identifiable underlying cause (Potschka et al.).
Some breeds are more genetically predisposed to idiopathic epilepsy, including Australian Shepherds and Labrador Retrievers, reinforcing the importance of breed-specific knowledge when evaluating seizure disorders (Mickelson & Steinberg).
Early diagnosis means earlier treatment and a better shot at long-term control.
4. Medications and Treatment Options for Canine Epilepsy
Once a diagnosis is made, the primary goal of treatment is to reduce seizure frequency and severity, ideally without affecting your dog’s quality of life. Most dogs with canine epilepsy start on antiepileptic drugs (AEDs), though each case may respond differently.
Common AEDs Used in Dogs
| Medication | Response Rate | Notes |
|---|---|---|
| Phenobarbital | 60–93% | First-line drug. Effective but may cause sedation, thirst, and liver enzyme elevation. |
| Potassium bromide | 50–70% | Used alone or with phenobarbital. It may take weeks to reach full effect. |
| Imepitoin | ~60% | Fewer side effects; suitable for mild to moderate idiopathic epilepsy (Charalambous et al.). |
| Levetiracetam | Variable | Often used in refractory cases or cluster seizures. Generally well-tolerated. |
Despite these options, about 30% of dogs experience refractory epilepsy, meaning their seizures remain uncontrolled even with standard AEDs (Hülsmeyer et al.).
Common Side Effects of Antiepileptic Drugs (AEDs)
While antiepileptic drugs are often life-changing for dogs with canine epilepsy, they aren’t without side effects. Most are manageable, especially with regular monitoring and dose adjustments.
- Sedation or Drowsiness: It’s common for dogs to appear groggy or sleepy when starting medications like phenobarbital or potassium bromide. This usually improves over time as their body adjusts.
- Increased Appetite and Weight Gain: AEDs can boost your dog’s hunger levels, sometimes significantly. Monitoring food portions and encouraging daily exercise can help prevent unwanted weight gain.
- Excessive Thirst and Urination (Polyuria/Polydipsia): Many dogs on phenobarbital or potassium bromide drink and urinate more often. If this becomes extreme or worsens suddenly, notify your vet; it could signal overmedication or a new issue.
- Liver Enzyme Elevation: Phenobarbital, in particular, can stress the liver over time. Your vet will likely recommend routine blood tests (every 6–12 months) to catch any changes early.
A tailored drug plan, developed in collaboration with your veterinarian or a veterinary neurologist, is key. What works for one dog may not work for another, and careful monitoring ensures your pet gets the benefits of seizure control without unnecessary side effects.
5. Living with Canine Epilepsy: Prognosis & Quality of Life

When your dog is diagnosed with canine epilepsy, one of the first questions is often: “What does this mean for their future?” The answer varies, but there’s a reason for hope. Many dogs with epilepsy live long, joyful lives with proper care and consistency.
Positive Prognostic Indicators
- Early response to the first prescribed AED
- Long seizure-free intervals (e.g., >6 months)
- Idiopathic epilepsy (vs. structural causes)
- Infrequent seizures at the time of diagnosis
Poorer Prognosis Linked To:
- Seizures that start before 6 months of age
- Cluster seizures (multiple within 24 hours)
- Status epilepticus (seizures lasting >5 minutes)
- No improvement after 3 months on medication
A long-term study showed that around 33% of dogs with idiopathic epilepsy achieved seizure remission, while 17% had poor outcomes, including euthanasia due to uncontrolled seizures (Wessmann et al.).
Still, with regular vet checkups, medication adjustments, and a proactive lifestyle, most dogs can enjoy a good quality of life despite canine epilepsy.
6. Practical Strategies to Manage Canine Epilepsy Daily
Daily life with canine epilepsy doesn’t have to feel like walking on eggshells. With structure and planning, you can help your dog stay safer and more stable, even during unpredictable episodes.
Routines Matter
Dogs with canine epilepsy benefit from a predictable routine:
- Feed at the same time each day.
- Give medications at exact intervals (use a reminder app).
- Maintain consistent sleep and activity patterns.
Avoid Common Triggers
Use your seizure diary to track environmental or emotional changes before seizures. Then, take steps to reduce known stressors like:
- Loud noises (use white noise machines during fireworks)
- Sudden schedule changes
- Intense excitement or vigorous exercise
Emergency Prep
Keep a seizure emergency kit at home:
- Rectal diazepam or intranasal midazolam (ask your vet)
- Towels and soft bedding
- Flashlight or headlamp (if seizures happen at night)
- Emergency contact list (vet, neurologist, nearby ER)
As Muñana et al. noted, many owners report high emotional distress, but education, preparation, and support networks help reduce anxiety.
With consistency and care, canine epilepsy can become a manageable part of your dog’s daily life.
7. FAQs About Canine Epilepsy
Here are answers to the most common questions dog owners ask about canine epilepsy, based on real clinical experience and current research.
❓ What is the most common cause of epilepsy in dogs?
The most common cause is idiopathic epilepsy, meaning there’s no identifiable brain abnormality. It’s likely genetic and typically appears in otherwise healthy dogs between 6 months and 6 years of age.
❓ Can dogs with canine epilepsy live a normal life?
Yes, many can. With appropriate medication, consistent routines, and seizure tracking, most dogs with canine epilepsy can enjoy long, fulfilling lives. Some even go seizure-free for years.
❓ How often will my dog have seizures?
This varies by case. Some dogs have only occasional seizures, while others may experience clusters. A well-documented seizure diary can help identify patterns and adjust treatment.
❓ Should I see a veterinary neurologist?
If your dog’s seizures are frequent, worsening, or not responding to initial treatment, a veterinary neurologist can help with advanced diagnostics and tailored polytherapy plans.
❓ What should I do during a seizure?
Stay calm. Move furniture away, cushion their head if possible, and time the seizure. Never place your hands in your dog’s mouth. If the seizure lasts more than 5 minutes, seek emergency care immediately.
Final Thoughts: There’s Hope for Dogs With Canine Epilepsy
A diagnosis of canine epilepsy can feel overwhelming, but it doesn’t have to be a life sentence. Many dogs with this condition continue to play, cuddle, and thrive for years with the right care.
Whether your dog has just had their first seizure or has been living with epilepsy for some time, remember: you’re not alone. There’s an entire community of dog owners, vets, and researchers working toward better treatments and brighter outcomes.
The key? Stay informed, track your dog’s patterns, follow a consistent treatment plan, and don’t hesitate to reach out for support, especially from a veterinary neurologist when needed.
With modern science, a little vigilance, and a lot of love, canine epilepsy can be managed, and your dog can still live their very best life.



![Read more about the article 5 proven Dogs Acupressure Points with Digestive Issues [Vet Guide]](https://doglifeexpert.com/wp-content/uploads/2025/07/ChatGPT-Image-Jul-14-2025-09_02_38-PM-300x200.png)

Pingback: IBD in Dogs: 5 Signs It’s Not Just a Food Sensitivity