🐾 Introduction
Canine Compulsive Disorders can be heartbreaking to witness—dogs trapped in endless cycles of tail-chasing, licking, pacing, or biting. As a small-animal vet in Ottawa, I’ve seen how these repetitive behaviors confuse and frustrate loving pet owners. What many don’t realize is that these actions aren’t bad habits—they’re clinical signs of a deeper, treatable condition.
Whether you’re noticing odd patterns in your dog’s behavior or already have a diagnosis, this guide will walk you through everything you need to know. Grounded in veterinary science and real-world practice, these seven insights will help you better understand, manage, and support your dog with canine compulsive disorders.
✅ Key Takeaways
- Canine compulsive disorders are repetitive behaviors like tail chasing, licking, or pacing that lack an obvious purpose and stem from stress, genetics, or brain chemistry.
- These behaviors must be distinguished from medical issues like pain, allergies, or neurological problems before a diagnosis is made.
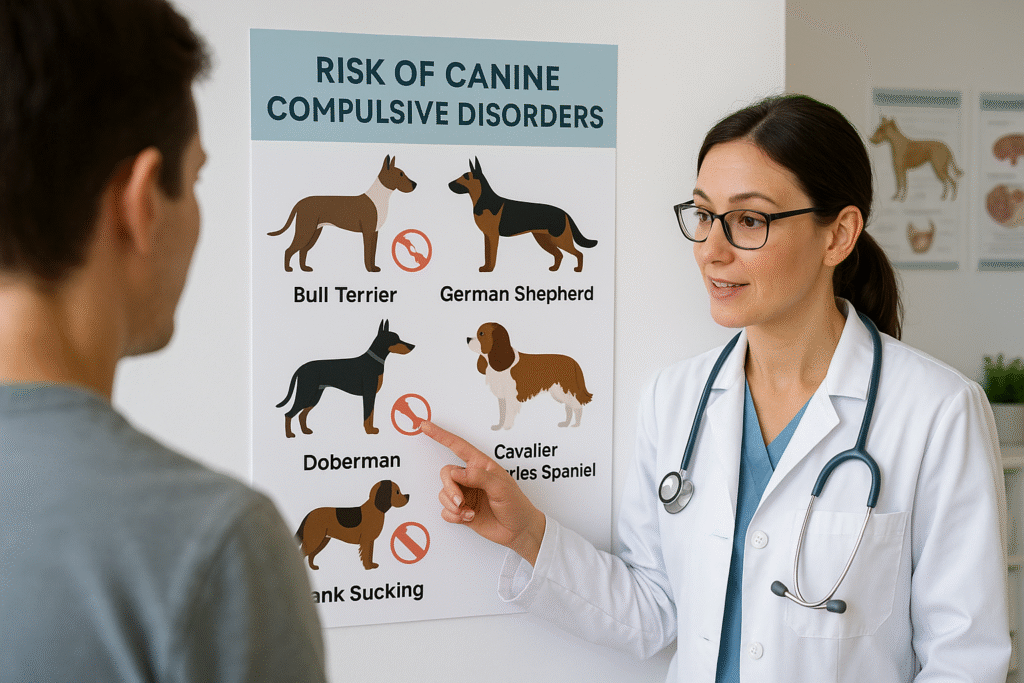
- Certain breeds—Bull Terriers, German Shepherds, Dobermans—are genetically predisposed.
- Treatment often involves medication (SSRIs or TCAs) paired with behavioral therapy to manage triggers and reduce severity.
- Early intervention and consistent owner education significantly improve the outlook for dogs living with canine compulsive disorders.
Table of Contents
1. Canine Compulsive Disorders Are More Common Than You Think
Canine compulsive disorders affect more dogs than many owners realize. Studies estimate that 2–5% of dogs seen by veterinary behaviorists display signs of compulsive behaviors (Contentful PDF). These behaviors can look like:
- Tail chasing until exhaustion or injury
- Paw licking that leads to acral lick dermatitis
- Flank sucking
- Shadow or light chasing
- Compulsive pacing or spinning
In my own practice, I’ve worked with clients whose dogs obsessively licked their paws raw. Initially suspected as allergies or infections, these cases were later diagnosed as canine compulsive disorders—revealing how easily these behaviors can be misread.
Most commonly, signs appear before the age of one, though many dogs don’t receive help until much later.
2. These Breeds Are Genetically Predisposed
Genetics play a strong role in canine compulsive disorders. Certain breeds have a higher risk due to inherited traits and neurochemical sensitivities. According to the AKC Canine Health Foundation, a gene located on canine chromosome 7 has been linked to compulsive behavior in dogs.
Breeds Frequently Affected:
| Breed | Common Compulsive Behavior |
|---|---|
| Bull Terriers | Tail chasing, flank sucking |
| German Shepherds | Spinning, chasing shadows |
| Dobermans | Flank sucking, blanket sucking |
| Cavalier King Charles Spaniels | Fly snapping, licking |
In one case, a young Bull Terrier presented with frequent, violent tail chasing that caused self-injury. Genetic risk, stress, and lack of mental enrichment all contributed to the compulsive cycle.
Recognizing breed predispositions allows for early monitoring and faster treatment of canine compulsive disorders—especially in high-risk puppies.
3. It’s Not Just Behavior—It’s Neurological
Canine compulsive disorders are not simply “bad habits” or disobedience—they’re linked to changes in the brain. Advanced imaging studies show abnormalities in the cortico-striato-thalamo-cortical circuits, a network also affected in human obsessive-compulsive disorder (OCD) (Contentful PDF).
Additionally, dogs with CD often have altered serotonin signaling, particularly reduced 5-HT2A receptor binding. This is why medications like fluoxetine (an SSRI) and clomipramine (a tricyclic antidepressant) are so effective in managing symptoms.
In my clinic, a Doberman named Luna showed flank sucking and pacing behaviors that dramatically improved after just three weeks on fluoxetine—clear evidence of the neurological underpinnings of her disorder.
Understanding that canine compulsive disorders are rooted in the brain—not simply behavior—helps owners take the condition seriously and approach it compassionately.
4. Accurate Diagnosis Requires Exclusion of Medical Conditions
Diagnosing canine compulsive disorders is a process of elimination. Many medical issues, such as skin infections, joint pain, or gastrointestinal discomfort, can mimic compulsive behaviors. Before confirming a diagnosis, your veterinarian must rule out these causes through physical exams, lab tests, and sometimes imaging (Clinician’s Brief).
Conditions That Mimic Canine Compulsive Disorders:
- Allergies causing excessive licking or chewing
- Pain from arthritis or injury triggering pacing or whining
- Neurological issues presenting as odd movements
- GI discomfort leading to obsessive grass eating or air licking
🏠 5-Minute Home Checklist
- Has this behavior become more frequent or intense?
- Does it happen across different environments and times?
- Is it interfering with sleep, play, or eating?
- Can you stop the behavior once it starts?
- Have any new stressors occurred recently (moves, routine change)?
A positive canine compulsive disorder diagnosis usually involves context-free, repetitive behaviors that persist despite redirection. As a veterinarian, I often ask owners to video their pet’s behavior at home to better understand triggers and patterns.
5. Medication Is Often Essential—But Not Alone
Medications play a vital role in treating canine compulsive disorders, particularly when behaviors are severe or self-injurious. The two most commonly prescribed drugs are:
🩺 Common Medications
| Drug | Class | Dosage Range | Notes |
|---|---|---|---|
| Fluoxetine | SSRI | 1–2 mg/kg once daily | Often well-tolerated; improvement seen in 1–3 weeks (Veterinary Evidence) |
| Clomipramine | TCA | 1–3 mg/kg twice daily | Can be equally effective; monitor heart function in at-risk dogs (Contentful PDF) |
Other medications like gabapentin or memantine may help dogs with seizure disorders or treatment-resistant symptoms.
In my experience, a German Shepherd with spinning behaviors did not improve until both fluoxetine and behavior therapy were introduced. Within two months, the behavior was manageable proving that meds alone are rarely a full solution for canine compulsive disorders.
💡 Important: Medication can take several weeks to show results, and side effects like sleepiness or appetite changes may occur early but usually resolve.

6. Behavior Therapy Completes the Puzzle
No medication can succeed alone without environmental and behavioral intervention. Dogs with canine compulsive disorders often react to stress, boredom, or frustration. By changing their environment and retraining responses, we can significantly reduce compulsion triggers.
🧠 Behavior Therapy Tools:
- Substitute actions: Teach calm commands like “sit” or “touch” to interrupt compulsive sequences.
- Environmental control: Block visual triggers (windows, lights, shadows), use crate training appropriately, and keep a consistent routine.
- Enrichment activities: Puzzle toys, scent work, daily walks, and structured play reduce mental tension.
- Avoid reinforcing: Don’t soothe or pet your dog during the compulsive behavior. This can unintentionally reward it (Cooperstown Veterinary Clinic).
In one case, I coached a family to redirect their Cavalier’s fly-biting episodes by rewarding calm sitting with a frozen Kong toy. Along with fluoxetine, her episodes dropped from daily to once every two weeks.
When appropriately managed, behavior therapy empowers both pet and owner in the battle against canine compulsive disorders.
7. Relapse Is Real—Prevention & Monitoring Matter
Even with treatment, dogs with canine compulsive disorders can relapse—especially during times of change, stress, or illness. Managing this condition is often a lifelong process, not a one-time cure.
🔄 What Triggers Relapse?
- Moving homes or changes in family dynamics
- Reduced exercise or enrichment
- Illness or pain resurfacing
- Inconsistent medication or training routines
As a vet, I recommend scheduling quarterly follow-ups for any dog diagnosed with canine compulsive disorders. These appointments help us adjust dosages, assess side effects, and track improvements or setbacks.
🧭 Managing Expectations
- Goal: Reduce the severity and frequency—not necessarily eliminate behaviors
- Celebrate progress (fewer episodes, shorter durations)
- Reinforce consistent routines and training
- Discuss long-term medication safety with your vet (DVM360)
By preparing for ups and downs, owners can create a stable and supportive environment that minimizes relapse risks and helps their dogs thrive.

❓ FAQ – Dog Owner Questions About Canine Compulsive Disorders
What are signs of canine compulsive disorders?
Look for repetitive behaviors that seem out of context or excessive, such as tail—chasing, licking, pacing, or staring at lights. If the behavior interferes with sleep, play, or eating, it may be a compulsive disorder.
Can canine compulsive disorders be cured?
Not usually. Most dogs experience significant improvement with treatment, but behaviors may not completely disappear. The goal is long-term management and improved quality of life.
Are some dogs born with it?
Yes. Genetics play a major role in canine compulsive disorders, especially in breeds like Bull Terriers, Dobermans, and German Shepherds.
What’s the best treatment?
A combination of medication and behavioral therapy works best. Starting treatment early improves outcomes and prevents worsening.
Will my dog need medication forever?
Not always, but many dogs benefit from long-term use. Your vet will monitor progress and determine if the dose can be reduced or stopped over time.




