Table of Contents
Introduction
If your dog has recently started drinking and peeing more than usual, seems hungrier than ever, or has developed a pot belly and thinning haircoat, you’re not alone, and you might be facing Cushing Disease in Dogs. As a Canadian veterinarian, I’ve diagnosed dozens of dogs with this hormonal condition, and while it can seem overwhelming at first, it’s very manageable with the right tools.
Cushing Disease in Dogs, also called hyperadrenocorticism, happens when the body produces too much cortisol, a stress hormone that, in excess, disrupts everything from your dog’s immune function to their metabolism. In 2025, we now have more precise diagnostics and safer, proven treatment options than ever before, which means earlier intervention and better outcomes for affected pets.
Let’s walk through the latest signs, tests, treatment strategies, and the real-world costs you should expect if your dog is diagnosed with Cushing Disease.
Medical Disclaimer
This article is for informational purposes only and does not replace professional veterinary advice, diagnosis, or treatment. Always consult your veterinarian if you suspect your pet may have a health condition. Never disregard or delay seeking veterinary care based on the information provided here.
Key Takeaways
- Cushing’s Disease in Dogs causes excess cortisol production, typically from a benign pituitary tumour (PDH) or, less commonly, an adrenal tumour.
- Common signs include increased thirst and urination, a pot-bellied abdomen, excessive hunger, thinning fur, and skin infections.
- Diagnosing Cushing’s requires bloodwork, urine tests, and confirmatory hormone testing like the ACTH stimulation or low-dose dexamethasone suppression test.
- Proven treatments in 2025 include trilostane (Vetoryl®) as first-line therapy, with mitotane or surgery as alternatives in select cases.
- Ongoing monitoring is critical to adjust medication doses and prevent side effects such as adrenal insufficiency.
- Treatment costs in Canada typically range from $150–$250/month for medication, plus periodic diagnostics and vet visits.
- With proper care, many dogs live 2–3 years or longer with a good quality of life.
What Is Cushing’s Disease in Dogs?
Also See: https://doglifeexpert.com/long-term-canine-atopic-dermatitis-management/
Cushing’s Disease in Dogs is a chronic endocrine condition where the adrenal glands produce too much cortisol. Cortisol is a vital hormone, helping the body manage stress, regulate metabolism, and support immune function. However, when produced in excess, it disrupts nearly every system in the body.
Causes of Cushing’s Disease
There are three main causes of Cushing’s Disease in Dogs:
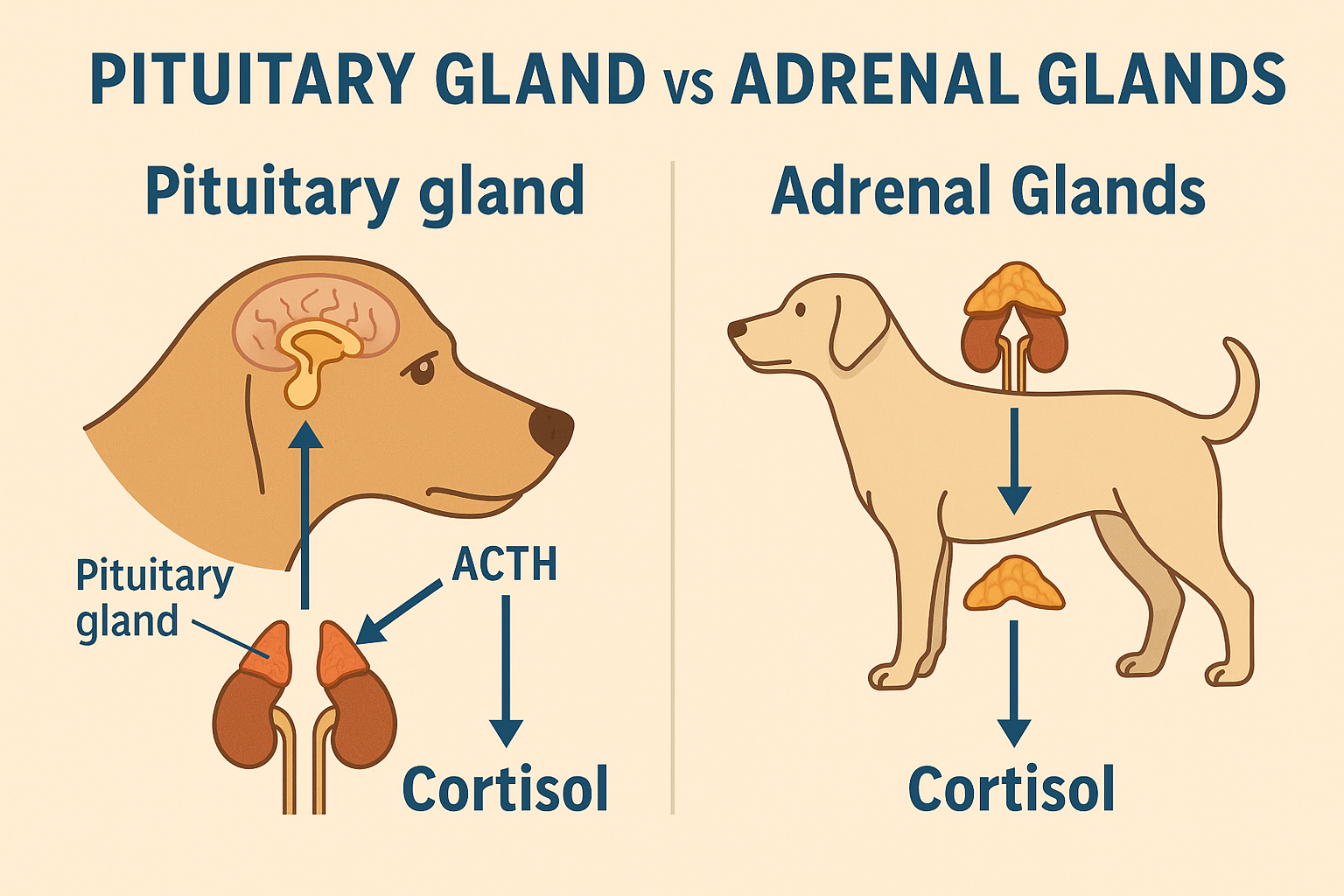
- Pituitary-dependent hyperadrenocorticism (PDH): This accounts for about 85% of cases. It’s caused by a benign tumour in the pituitary gland that overstimulates the adrenal glands to release cortisol.
- Adrenal-dependent Cushing’s: Caused by a tumour on one of the adrenal glands. These can be benign or malignant, and surgery is often considered.
- Iatrogenic Cushing’s: This occurs when dogs receive prolonged or high-dose corticosteroid treatment for other conditions, leading to cortisol overexposure.
Which Dogs Are at Risk?
- Most cases occur in middle-aged to senior dogs, typically over six years old.
- Breeds more prone to Cushing’s Disease in Dogs include:
- Poodles
- Dachshunds
- Beagles
- Boxers
- Yorkshire Terriers
Some studies also suggest a higher incidence in females and neutered dogs, though this can vary by population.
Learn more from the Merck Veterinary Manual
Signs of Cushing’s Disease in Dogs

The clinical signs of Cushing’s Disease in Dogs often develop gradually, which is why they’re sometimes mistaken for “normal ageing.” However, early recognition can make a significant difference in diagnosis and long-term care.
Most Common Clinical Signs
- Increased thirst and urination (PU/PD) – seen in over 90% of cases
- Excessive hunger (polyphagia) affects about 75–80% of dogs
- Panting often occurs even at rest or in cool environments
- Lethargy and muscle weakness
- Pot-bellied appearance – due to abdominal muscle loss and fat redistribution
PetMD explains these signs in detail
Skin and Coat Changes
Cortisol excess affects skin integrity and hair growth, leading to:
- Thinning or patchy haircoat
- Recurrent skin infections
- Blackheads (comedones)
- Thinning skin that bruises easily
- Calcinosis cutis – rare, but distinctive, firm white plaques under the skin
Secondary Complications
If left untreated, Cushing Disease in Dogs can also lead to:
- Urinary tract infections – often without symptoms
- Diabetes mellitus – due to cortisol-induced insulin resistance
- Hypertension (high blood pressure)
- Pancreatitis
- Proteinuria or kidney damage
According to IDEXX’s endocrine diagnostics guide, early testing is essential if these signs are present.
How Is Cushing Disease Diagnosed?

Diagnosing Cushing’s Disease in Dogs can be challenging because the symptoms often overlap with other conditions. A methodical approach, starting with general tests and moving toward more specific hormone testing, is key.
Step 1: Initial Screening Tests
Your vet will usually begin with:
- Complete blood count (CBC)
- Serum biochemistry profile elevated alkaline phosphatase (ALP), cholesterol, and glucose, are common
- Urinalysis often reveals dilute urine and may show signs of urinary tract infection
These help rule out other illnesses and raise suspicion for Cushing Disease in Dogs. Learn more in IDEXX’s cortisol testing guide.
Step 2: Hormonal Testing
Once initial findings point toward hyperadrenocorticism, your vet may recommend one or more of the following:
ACTH Stimulation Test
- Measures cortisol before and after injection of synthetic ACTH
- Dogs with Cushing Disease often show exaggerated cortisol production
- Commonly used to confirm diagnosis and to monitor treatment with trilostane
- PetMD outlines how this test is interpreted
Low-Dose Dexamethasone Suppression Test (LDDST)
- Cortisol levels are measured at baseline, 4 hours, and 8 hours after a low dose of dexamethasone
- In healthy dogs, cortisol is suppressed; in Cushing dogs, it remains elevated
- More sensitive than the ACTH test, but also more likely to give false positives
Read how LDDST fits into the full diagnostic picture via the Merck Veterinary Manual
Step 3: Differentiating PDH from Adrenal Tumours
After confirming Cushing Disease in Dogs, it’s important to determine the cause:
- High-Dose Dexamethasone Suppression Test (HDDST): if cortisol levels drop, PDH is likely; if not, an adrenal tumour is suspected
- Endogenous ACTH measurement high = PDH, low = adrenal tumour
- Abdominal ultrasound helps identify adrenal masses or changes
- CT or MRI is used in referral centres to visualise pituitary masses
Dechra Veterinary Products offers a complete visual guide to testing protocols
Treatment Options for Cushing Disease in Dogs

In 2025, treatment for Cushing’s Disease in Dogs is more effective and safer than ever, with both medical and surgical options tailored to the underlying cause and your dog’s overall health.
Trilostane (Vetoryl) – First-Line Therapy
Trilostane is the only Health Canada- and FDA-approved drug for treating both pituitary and adrenal-dependent Cushing’s. It works by reversibly blocking cortisol production, offering safer control than older drugs like mitotane.
- Starting dose: ~2 mg/kg once daily, adjusted as needed
- Benefits: Reversible, well-tolerated, effective in controlling PU/PD, appetite, and coat issues
- Side effects: Lethargy, vomiting, diarrhoea, appetite loss, most are mild and dose-responsive
- Monitoring: ACTH stimulation test 10–14 days after starting, then at 1 month, then every 3 months
According to AAHA’s monitoring guidelines, regular follow-ups are key to avoiding side effects like Addisonian crisis.
Dechra provides dosing and safety data on Vetoryl here
Mitotane (Lysodren) – Potent But Riskier
Mitotane is an older chemotherapy-type drug that destroys adrenal cortex tissue, used mainly in pituitary-dependent cases.
- Loading phase: 40–100 mg/kg/day for ~5–25 days
- Maintenance: 30–50 mg/kg/week
- Risks: Vomiting, lethargy, diarrhoea, permanent adrenal insufficiency (~2–5%)
It’s generally reserved for cases where trilostane fails or isn’t tolerated. Learn more in the VIN canine Cushing’s treatment guide
Selegiline (Anipryl) – Niche Use
Approved for PDH-related Cushing’s, selegiline inhibits dopamine metabolism, reducing ACTH output from the pituitary. However, it’s far less effective than trilostane.
- Success rate: ~20% in select cases
- Best used: For early or mild PDH, or if owners decline more intensive therapy
- Today’s Veterinary Practice reviews its limited use
Surgery and Radiation – Speciality Centre Options
- Hypophysectomy (pituitary removal) offers a potential cure but is only performed at advanced referral hospitals. Survival at 4 years post-op is ~72–79%
- Adrenalectomy for adrenal tumours depends on the tumour size and spread
- Radiation therapy for non-surgical PDH cases is slow to act, costly, and requires multiple sessions
ScienceDirect’s review outlines surgical outcomes
Monitoring & Long-Term Prognosis

Managing Cushing’s Disease in Dogs doesn’t end with a diagnosis or starting treatment. Ongoing monitoring and adjustments are essential to ensure your dog remains comfortable, stable, and safe.
What Owners Should Monitor at Home
Keeping track of your dog’s day-to-day behaviour and physical changes is essential for safely managing Cushing’s Disease in Dogs. Here’s what to look for between vet visits:
- Water Intake – Measure how much your dog drinks daily. Sudden increases or drops could signal under- or over-treatment. A general guideline: more than 100 mL/kg/day is excessive.
- Appetite – While most Cushing’s dogs are ravenous, a sudden decrease in appetite can indicate cortisol suppression (possibly from too much trilostane). Monitor closely after dose changes.
- Urination Habits – Increased urination or urinary accidents in a previously house-trained dog often persist early in treatment. A reduction may indicate improvement or, if too drastic, Addisonian risk.
- Energy & Mobility – Is your dog more energetic, playful, or less lethargic compared to before starting treatment? Improvement is a good sign. Limping or stiffness could suggest unrelated issues.
- Skin & Coat – Keep an eye on new bald patches, slow-healing sores, or return of skin infections. These may need topical care or signal poor hormonal control.
- Panting & Discomfort – Persistent panting, especially at night or during rest, can indicate ongoing cortisol excess or internal stress. New signs like pacing, restlessness, or whining warrant a check-up.
Tip: Keep a weekly log of these observations and bring it to follow-ups. Even minor patterns can help your vet fine-tune treatment for Cushing’s Disease in Dogs. Treatment or disease progression. Keep a log and share it with your veterinarian during follow-ups.
Veterinary Monitoring Schedule
According to VetGirl’s clinical blog:
- Initial trilostane follow-up: ACTH stimulation test 10–14 days after starting
- Second recheck: ~30 days
- Ongoing checks: Every 3–6 months, or sooner if symptoms change
- Tests at each visit: ACTH stim, electrolytes, liver values, physical exam
Expected Lifespan
With good care, dogs with pituitary-dependent Cushing’s treated with trilostane typically live 2 to 3 years post-diagnosis, sometimes longer. Dogs with adrenal tumours may live 1 to 2 years, especially if surgery is not an option.
The FDA outlines average outcomes and drug safety here
5-Minute Home Checklist: Could Your Dog Have Cushing’s?
If you’re worried your dog may have Cushing’s Disease, use this quick checklist. It’s not a diagnosis, but it helps you decide whether to schedule a vet visit.
✅ Watch for These Symptoms
| Symptom | Present? |
|---|---|
| Drinking more water than usual | ☐ Yes ☐ No |
| Urinating more frequently | ☐ Yes ☐ No |
| Increased hunger | ☐ Yes ☐ No |
| Bloated or pot-bellied abdomen | ☐ Yes ☐ No |
| Hair loss or a thinning coat | ☐ Yes ☐ No |
| Lethargy or muscle weakness | ☐ Yes ☐ No |
| Excessive panting | ☐ Yes ☐ No |
| Recurrent skin or ear infections | ☐ Yes ☐ No |
| Unexplained weight gain | ☐ Yes ☐ No |
| Thinning skin or easy bruising | ☐ Yes ☐ No |
What to Do
If you checked 3 or more boxes, especially PU/PD (increased thirst and urination), book a vet exam. Cushing’s Disease in Dogs is manageable, but earlier intervention leads to better results.
For additional guidance, consult Long Beach Animal Hospital’s symptom breakdown
Prevention & Risk Reduction

While not all cases of Cushing’s Disease in Dogs can be prevented, especially those linked to pituitary or adrenal tumours, some forms can be avoided or better managed with early intervention.
Preventing Iatrogenic Cushing’s
The iatrogenic form of Cushing’s arises from long-term corticosteroid use, such as prednisone or dexamethasone, often prescribed for allergies, autoimmune issues, or chronic inflammation.
Tips to Reduce Risk:
- Never give steroids without veterinary oversight
- Use the lowest effective dose for the shortest time
- Switch to non-steroidal options (e.g., Apoquel®, Cytopoint®, Atopica®) when appropriate
- Schedule rechecks for chronic steroid users at least every 3–6 months
- Monitor for early signs: PU/PD, skin changes, or increased appetite
The FDA’s canine health advisory also encourages avoiding over-reliance on steroids for chronic conditions.
FAQs About Cushing’s Disease in Dogs
Can dogs live with untreated Cushing’s?
Some dogs may survive for months or even a few years without treatment, but most will experience progressive symptoms muscle wasting, infections, diabetes, or high blood pressure. Untreated Cushing’s Disease in Dogs significantly reduces quality of life and increases the risk of complications.
How fast does Cushing’s Disease progress?
It varies. In many cases, symptoms develop gradually over months to years. However, once clinical signs become noticeable, progression can accelerate. A diagnosis may be delayed for up to 8 months after the first subtle symptom appears.
Do dogs with Cushing’s suffer?
Not necessarily, especially if the condition is diagnosed early and managed properly. Dogs on trilostane often regain energy, normalise their appetite, and show coat improvement within a few weeks. Without treatment, however, complications like UTIs, pancreatitis, or painful skin infections can develop.
What are red-flag side effects of trilostane?
Warning signs of over-suppression include vomiting, diarrhoea, lethargy, poor appetite, and collapse. These may indicate Addisonian crisis, requiring immediate vet care. Monitoring ACTH levels helps avoid this outcome.
Dechra’s trilostane monitoring guide emphasises early detection of dosing problems.
Can Cushing’s Disease be cured?
- Pituitary-dependent cases: Not cured, but controlled long-term with trilostane
- Adrenal-dependent cases: May be cured with successful adrenalectomy
- Iatrogenic cases: Reversible once steroid use is tapered (under supervision)
ScienceDirect’s treatment overview highlights surgical success rates and outcomes.
Typical Costs of Treating Cushing’s Disease in Dogs (Canada)
In Canada, managing Cushing’s Disease in Dogs involves both initial diagnostic expenses and ongoing treatment costs. These can vary widely depending on location, size of dog, and treatment choice.
Cost Table: 2025 Averages in Canadian Clinics
| Category | Estimated Cost (CAD) |
|---|---|
| Initial blood/urine panel | $150 – $250 |
| ACTH stimulation or LDDST | $250 – $350 |
| Abdominal ultrasound | $400 – $700 |
| CT or MRI (referral only) | $1,500 – $2,500 |
| Trilostane (Vetoryl®) monthly | $120 – $250 depending on dog’s weight |
| ACTH recheck (every 3–6 months) | $200 – $350 |
| Mitotane treatment (loading + maintenance) | $200 – $500/month |
| Adrenalectomy surgery | $3,000 – $7,000 (referral centres only) |
| Radiation therapy (PDH) | $5,000 – $10,000+ (multi-session) |
Budgeting Tips
- Request medication quotes from compounding pharmacies for potential savings.
- Use pet insurance to offset the cost of diagnostics and treatment. Many plans cover endocrine disorders if diagnosed after enrollment.
- Some clinics offer endocrine packages or care plans for chronic management.
Even with monthly costs, most owners find that the improved quality of life and symptom control in their dogs make the investment worthwhile.
For more, see IDEXX’s 2025 endocrinology resources
Final Thoughts
Cushing’s Disease in Dogs can be a life-altering diagnosis, but it’s far from a hopeless one. With modern diagnostics and treatment options like trilostane, most dogs can regain a good quality of life and enjoy months to years of stability when monitored carefully.
As a veterinarian, I’ve seen dogs go from panting, lethargic, and balding to bright, energetic, and playful again with just a few weeks of properly adjusted treatment. Early recognition, consistent monitoring, and good communication with your veterinary team are your best tools for managing this condition.
Whether your dog is showing symptoms or is already diagnosed, don’t panic. There’s a well-established path forward, and in 2025, it’s better informed, safer, and more effective than ever.