Medical Disclaimer: This content is for informational purposes only and is not a substitute for professional veterinary advice, diagnosis, or treatment. Always consult your veterinarian regarding your dog’s specific health needs especially when managing chronic kidney disease in dogs.
Table of Contents
Introduction
If your dog has been diagnosed with chronic kidney disease, you’re not alone, and you’re not powerless. As a veterinarian, I’ve worked with countless pet owners navigating this diagnosis. It can feel overwhelming at first, but with early care and the right tools, chronic kidney disease in dogs can often be managed successfully for months or even years.
By definition, chronic kidney disease (CKD) involves the gradual, irreversible loss of kidney function over time, typically diagnosed after persistent signs for at least three months, including elevated creatinine and urea levels in bloodwork (PubMed). The condition affects a dog’s ability to filter toxins, regulate hydration, and balance electrolytes. Left unmanaged, CKD leads to weight loss, nausea, inappetence, and eventually a decline in quality of life.
The goal of managing chronic kidney disease in dogs isn’t to reverse the damage because that’s not possible, but to slow progression and preserve comfort. Thankfully, research shows that a comprehensive plan that includes a therapeutic renal diet, medications like phosphate binders, appetite stimulants, hydration support, and regular monitoring can significantly extend both life and quality of life.
This guide walks you through the evidence-based strategies that veterinarians like me use to manage chronic kidney disease in dogs in daily practice. Whether your dog is newly diagnosed or already on treatment, you’ll find clear, practical advice rooted in current veterinary guidelines, including those from IRIS (International Renal Interest Society) and DVM360.
Key Takeaways
- Chronic kidney disease in dogs is a progressive, lifelong condition that requires early intervention to slow its progression and preserve quality of life.
- A therapeutic renal diet is proven to reduce uremic episodes and increase survival time in dogs with CKD.
- Common treatments include phosphate binders, appetite stimulants, antiemetics, blood pressure medications, and subcutaneous fluids.
- Dogs with CKD need routine monitoring every 3–4 months, including bloodwork, urine testing, and blood pressure measurements.
- Working closely with your veterinarian helps tailor a plan based on CKD stage and your dog’s response.
- While not curable, chronic kidney disease in dogs can often be managed for months or even years with consistent, proactive care.
What Is Chronic Kidney Disease in Dogs?
Also see: https://doglifeexpert.com/7-natural-remedies-for-dog-skin-allergies/
Chronic kidney disease in dogs refers to a sustained, irreversible loss of kidney function over time, typically diagnosed when renal abnormalities persist for over 3 months. Unlike acute kidney injury, which develops suddenly and may be reversible, CKD is progressive and incurable (PubMed).
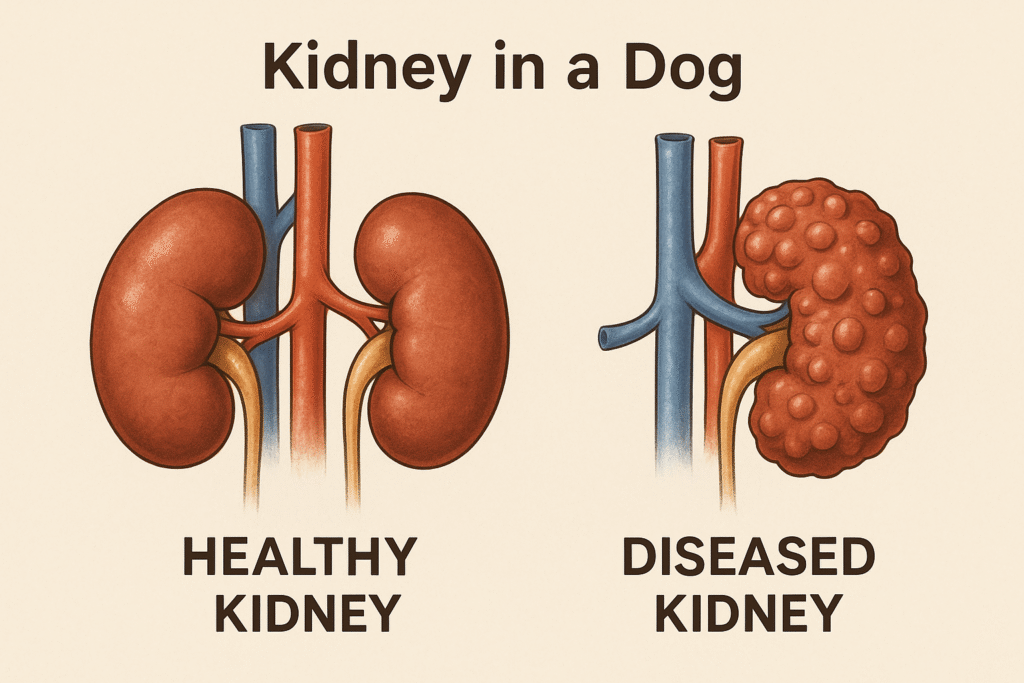
In a healthy dog, the kidneys filter waste, regulate electrolytes, maintain hydration, and help control blood pressure. But with CKD, damaged nephrons (the kidney’s filtering units) can’t be regenerated. As kidney function declines, waste products like creatinine, urea, and phosphorus accumulate in the bloodstream, leading to systemic effects.
Most dogs are diagnosed at IRIS Stage 2 or 3, when blood creatinine exceeds 1.4 mg/dL and clinical signs begin to emerge (Wiley Online Library). IRIS staging guides treatment and monitoring frequency, with staging based on serum creatinine, SDMA, urine protein levels, and blood pressure.
Common Signs of CKD in Dogs
- Increased thirst (polydipsia) and urination (polyuria)
- Loss of appetite
- Weight loss and muscle wasting
- Nausea or vomiting
- Bad breath (uremic halitosis)
- Lethargy
- Dehydration
It’s not uncommon for chronic kidney disease in dogs to be diagnosed incidentally during routine bloodwork, especially in senior pets. That’s why regular wellness exams are vital for early detection, because the earlier CKD is caught, the better the outcome (DVM360).
Why Early Management Matters
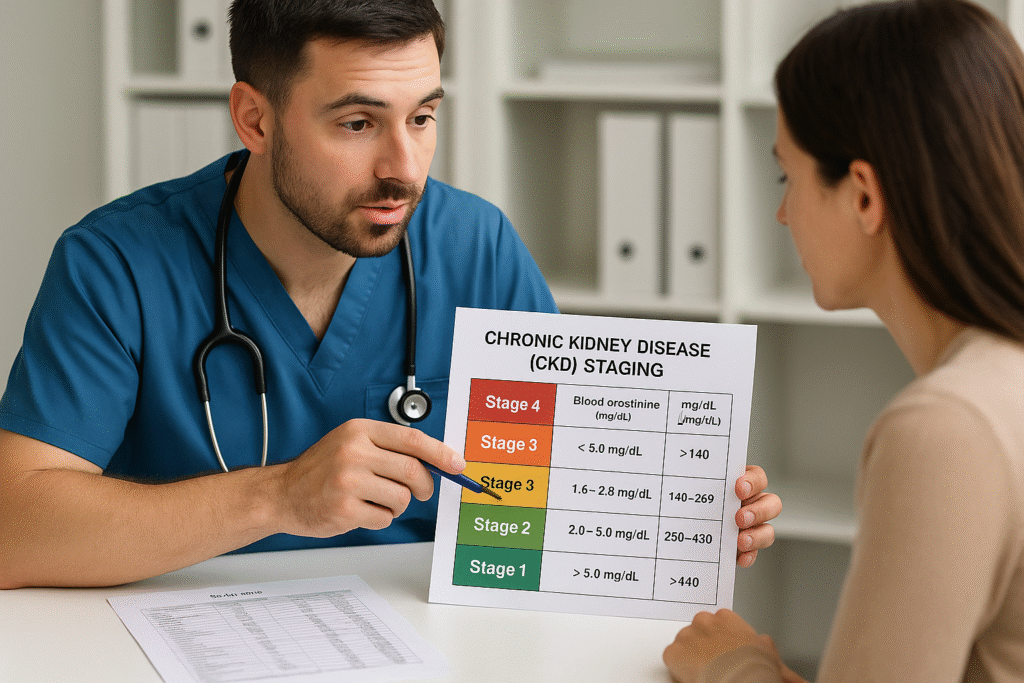
Early detection of chronic kidney disease in dogs can dramatically improve outcomes. Unfortunately, many dogs aren’t diagnosed until IRIS Stage 2 or later, when about 66% of nephrons may already be compromised. At this point, serum creatinine often exceeds 1.4 mg/dL, and symptoms like decreased appetite or vomiting may start to appear (Wiley Online Library).
Why does this timing matter? Because the earlier we intervene with diet, medications, and hydration, the better we can:
- Slow the loss of kidney function
- Delay onset of uremic symptoms
- Stabilize body condition
- Improve quality of life
- Extend survival time (PubMed, DVM360)
One landmark study published in Today’s Veterinary Practice found that dogs on a therapeutic renal diet lived nearly twice as long as dogs on maintenance food. That means time, often years, spent feeling better and enjoying life with their families (Today’s Veterinary Practice).
If you’ve just received a CKD diagnosis, know that you have a window of opportunity. Acting early helps minimize complications like hypertension, phosphorus buildup, and acid–base imbalance, all of which worsen CKD progression. It’s not just about adding time, but quality time, to your dog’s life.
Nutritional Therapy: Renal Diets for Dogs

Ask any vet what the most important intervention is for chronic kidney disease in dogs, and we’ll likely say: nutrition. Therapeutic renal diets aren’t just supportive, they’re scientifically proven to slow disease progression, reduce uremic episodes, and extend survival (Today’s Veterinary Practice).
What Makes a Renal Diet Special?
Renal diets are carefully formulated to reduce the metabolic workload on damaged kidneys while still meeting a dog’s nutritional needs. Key features include:
- Restricted but high-quality protein: Limits nitrogenous waste, which the kidneys must excrete, without causing muscle wasting.
- Low phosphorus: Elevated phosphorus contributes to further nephron damage. Dietary restriction helps maintain phosphorus <4.6 mg/dL in early stages (The Spruce Pets).
- Reduced sodium: Helps manage blood pressure.
- Increased omega-3 fatty acids: From fish oil, these may reduce glomerular inflammation.
- Alkalinizing agents: Buffers like potassium citrate reduce metabolic acidosis, which worsens with CKD.
- Soluble fibre: Supports uremic toxin excretion through the colon (DVM360).
Transitioning to a Renal Diet
Dogs with chronic kidney disease often have poor appetite, so a diet change can be a challenge. Transition gradually over 7–10 days:
- Start by mixing 25% renal diet with 75% current food.
- Increase renal diet every 2–3 days.
- Warm canned food slightly to enhance the aroma.
- Offer small, frequent meals in a calm setting.
If your dog still won’t eat, consider appetite stimulants (like mirtazapine or capromorelin), or in advanced cases, a feeding tube (esophagostomy or gastrostomy) to maintain calorie intake (nbflanes.com).
Commercial vs. Home-Cooked Diets
Veterinary-prescribed brands like Hill’s k/d, Royal Canin Renal, or Purina NF are balanced and proven. Home-cooked renal diets must be formulated with a veterinary nutritionist. Improper calcium-phosphorus ratios or vitamin deficiencies can worsen CKD.
Ultimately, diet is the single most impactful intervention for chronic kidney disease in dogs. If your dog eats the renal food reliably, you’re already winning a huge part of the battle.
Medication and Supplement Support

While diet forms the cornerstone of treatment, medications and supplements are often essential for managing the systemic effects of chronic kidney disease in dogs. These help control phosphorus, blood pressure, nausea, and other complications.
Phosphate Binders
Even the best renal diets may not lower blood phosphorus enough. That’s where phosphate binders come in. Given with meals, they attach to dietary phosphorus in the gut and reduce absorption, keeping serum phosphorus ideally below 4.6 mg/dL (The Spruce Pets).
Common options:
- Aluminum hydroxide (non-prescription)
- Lanthanum carbonate
- Epakitin or Renalzin (nutraceuticals)
Appetite Stimulants and Antiemetics
Dogs with CKD often feel nauseated, leading to food refusal and weight loss. Appetite stimulants or anti-nausea meds may help:
- Mirtazapine (oral or transdermal): Boosts appetite and reduces nausea.
- Capromorelin (Entyce): A ghrelin receptor agonist that encourages eating.
- Maropitant (Cerenia) and ondansetron: Reduce vomiting and nausea (PetMD).
Anti-Hypertensives
High blood pressure (hypertension) both worsens and results from chronic kidney disease in dogs. Treating it is crucial to protect the remaining kidney function.
- ACE inhibitors (e.g., enalapril, benazepril): Lower pressure in the kidney’s filtering system.
- Amlodipine may be added for systemic hypertension.
Blood pressure should be checked regularly; the target is often <140 mmHg systolic (Veterinary Partner).
Other Supplements
Depending on lab results, your vet may prescribe:
- Potassium supplements: For dogs with hypokalemia
- Calcitriol or vitamin D analogs: To correct renal secondary hyperparathyroidism
- Antacids (e.g., famotidine): For acid reflux or GI ulcers
- Erythropoietin-stimulating agents: For anemia in advanced CKD (nbflanes.com)
Every drug choice should consider reduced renal clearance. Dosing errors can worsen outcomes, so always consult your veterinarian or use published dosing guidelines for CKD patients.
These medications and supplements, when used thoughtfully, can help your dog feel better, eat better, and maintain stable lab values over time.
Hydration Strategies for Dogs with CKD

One of the biggest challenges in chronic kidney disease in dogs is maintaining proper hydration. Damaged kidneys can’t concentrate urine effectively, leading to excessive fluid loss through frequent urination, known as polyuria. Dogs try to compensate by drinking more (polydipsia), but over time, this often isn’t enough.
Why Hydration Matters
Hydration plays a critical role in:
- Diluting uremic toxins
- Supporting blood flow to the remaining nephrons
- Preventing dehydration and electrolyte imbalances
- Enhancing appetite and energy levels
How to Support Hydration at Home
1. Wet Food or Soaked Kibble
Feeding canned renal diets adds water by default. If using dry kibble, soak it in warm water or unsalted broth to increase moisture intake (The Spruce Pets).
2. Add Water to Every Meal
Even canned food can be watered down further. Offer multiple water bowls around the house, and refresh them often to encourage drinking.
3. Subcutaneous Fluids (SubQ Fluids)
In more advanced stages, many owners learn to give subcutaneous fluids at home, typically lactated Ringer’s solution 2–3 times per week or as directed by their vet. This is one of the most effective ways to maintain hydration when oral intake is insufficient (PetMD).
Your veterinarian can teach you how to safely give fluids under the skin. It may sound intimidating, but many owners find it surprisingly simple with practice, and it can dramatically improve your dog’s energy and comfort.
I’ve seen dogs with chronic kidney disease perk up within hours of their first fluid session. It’s one of the most empowering tools you can learn as a caregiver.
Monitoring CKD: Labwork and BP

Ongoing monitoring is just as important as the initial treatment plan for chronic kidney disease in dogs. Because CKD is progressive, your dog’s needs will change over time, and we can only adjust care appropriately if we’re tracking the right parameters.
What Should Be Monitored?
Veterinarians typically recheck CKD patients every 3–4 months (or more often for advanced stages). Each visit may include:
- Serum creatinine and SDMA: Gauge filtration rate
- BUN (blood urea nitrogen): Reflects protein metabolism
- Phosphorus and calcium: High phosphorus accelerates nephron loss
- Potassium levels: Important for muscle and cardiac function
- Hematocrit/PCV: Screens for anemia
- Urinalysis and urine protein: creatinine ratio (UPC): Helps stage CKD
- Blood pressure: Essential for spotting and treating hypertension early (DVM360)
Even if your dog looks stable, lab values can shift significantly between visits. For instance, phosphorus may creep upward silently, which could call for starting phosphate binders or adjusting the diet.
Adjusting the Plan
Every check-up helps refine your dog’s care. Based on lab trends and how your dog’s doing clinically, your vet might:
- Adjust medications or dosages
- Add supplements like potassium or vitamin D
- Increase subQ fluid frequency
- Recommend further imaging (e.g., abdominal ultrasound)
- Shift to a different renal diet if the appetite drops
From my experience, the dogs who live longest with chronic kidney disease aren’t always the ones with perfect lab values; they’re the ones whose caregivers stay consistent with check-ins and communication.
Life Expectancy and Prognosis

The prognosis for chronic kidney disease in dogs varies widely, depending on the stage of disease, how early it’s diagnosed, and how consistently it’s managed. While CKD isn’t curable, many dogs can live comfortably for months or even years with the right support.
How Long Can a Dog Live With CKD?
- IRIS Stage 1 or early Stage 2: Dogs may live several years with proper care.
- Stage 3: Many live 6–24 months, depending on clinical signs and response to treatment.
- Stage 4: Prognosis is more guarded, often weeks to months, though some dogs exceed expectations with intensive support (PubMed).
A 2021 study found that dogs eating a veterinary renal diet lived significantly longer than those on standard food. Quality of life was also better, with fewer uremic crises and hospitalizations (nbflanes.com).
Maintaining Body Condition
Body condition is a key predictor of survival in chronic kidney disease in dogs. Dogs that become underweight or muscle-wasted fare worse over time.
Aim for a body condition score (BCS) of 4–5 out of 9. If your dog is losing weight:
- Adjust caloric intake or feeding frequency
- Add appetite stimulants
- Discuss feeding tubes if oral intake drops too low
In my practice, I’ve seen several older dogs gain back weight and energy after implementing appetite support and increasing fluid therapy.
Quality of Life Matters Most
Even when prognosis is limited, symptom control is achievable. Nausea, dehydration, high phosphorus, and hypertension can all be managed with the right plan. Your vet may use tools like quality-of-life scoring charts to help guide decisions as the disease progresses.
The bottom line? Chronic kidney disease in dogs is rarely a short-term death sentence. With vigilance and tailored care, many dogs go on to have happy, comfortable lives.
Real-World Tips for Pet Parents

Managing chronic kidney disease in dogs can feel overwhelming, especially at first. But over time, many owners become confident, effective caregivers. Here are practical, veterinarian-approved tips to help you and your dog thrive through this journey.
Partner With Your Veterinarian
Your vet is your biggest ally. CKD management isn’t “set it and forget it” your dog’s needs will evolve. Stay in close contact, and don’t hesitate to ask questions or request changes to the treatment plan.
Feed the Best Diet Your Dog Will Eat
- Renal diets are ideal, but only if your dog eats them.
- Try warming food, hand-feeding, or adding low-sodium broth.
- If appetite is low, discuss stimulants or even a feeding tube.
- Never force-feed; it may worsen food aversion.
Stay Consistent With Meds and Fluids
- Give phosphate binders with meals; timing matters.
- Keep a medication chart or app to stay on schedule.
- If using subcutaneous fluids, stick to the recommended volume and frequency.
- Ask your vet about rotating injection sites to avoid discomfort.
Track Appetite, Weight, and Energy
Small changes matter. If your dog skips meals, seems more tired, or loses weight, that’s a signal to recheck labs or tweak the plan.
Stay on Top of Monitoring
Don’t skip check-ups, even if your dog seems “fine.” Many changes occur silently in CKD. Proactive labwork helps prevent sudden downturns.
Communicate Promptly
Any signs of vomiting, diarrhea, refusal to eat, or lethargy should be reported immediately. Early intervention can make the difference between a minor adjustment and a crisis.
In the real world, managing chronic kidney disease in dogs is a balancing act. You’ll have great days and hard ones. But consistency, compassion, and teamwork with your vet go a long way in giving your dog the best quality of life possible.
FAQs About Chronic Kidney Disease in Dogs
1. What causes chronic kidney disease in dogs?
CKD often results from age-related wear, genetic predisposition (e.g., in Shih Tzus or Cocker Spaniels), chronic infections, or previous kidney injury. In many cases, the exact cause of chronic kidney disease in dogs remains unknown.
2. Is chronic kidney disease in dogs painful?
Not directly, but the side effects like nausea, dehydration, ulcers, or electrolyte imbalances can be uncomfortable. Pain management isn’t usually required, but symptom relief (anti-nausea meds, fluids) dramatically improves comfort.
3. Can a dog recover from chronic kidney disease?
No. CKD is irreversible. However, dogs can often live well for months to years with early diagnosis, a renal diet, hydration, medications, and frequent monitoring.
4. How often should a dog with CKD see the vet?
Typically, every 3–4 months for exams, labwork, and medication reviews. More frequent visits may be needed if the disease progresses or symptoms flare.
5. Can I give home-cooked meals instead of prescription renal diets?
Yes, but only if the diet is formulated by a veterinary nutritionist. Improper nutrient balance can worsen chronic kidney disease in dogs. Commercial renal diets are preferred due to their proven safety and effectiveness.
Final Thoughts
Living with a dog who has kidney disease isn’t easy, but it’s far from hopeless. Chronic kidney disease in dogs can be managed successfully with a combination of the right diet, medication, hydration, and ongoing veterinary care.
If your dog was just diagnosed, take a deep breath. You now have a roadmap. Start with a therapeutic renal diet, discuss supplements like phosphate binders or appetite stimulants, and learn how to monitor your dog’s weight, labs, and comfort at home. Don’t hesitate to ask your vet about options like subcutaneous fluids or feeding support if appetite wanes.
In my experience, dogs with CKD often surprise us. With consistent care and a bit of patience, many enjoy happy, meaningful years beyond their diagnosis. You’re your dog’s best advocate, and every small adjustment you make matters more than you think.





Pingback: 5 Proven Treatments That Stabilize Diabetes in Dogs