Medical Disclaimer: This article is for informational purposes only and does not constitute medical advice. If you believe your dog is showing signs of IMHA, contact your veterinarian or an emergency animal hospital immediately.
From my years in clinical practice, few diagnoses can make a pet owner’s world stop as suddenly as Immune-Mediated Hemolytic Anemia, or IMHA. One day your dog is fine; the next, they are fighting for their life. This disease is a true emergency, where the body’s own defences turn against itself with devastating speed. But understanding this complex condition is the first step toward fighting back.
Key Takeaways
Immune-Mediated Hemolytic Anemia (IMHA) is a serious autoimmune disease where a dog’s immune system mistakenly destroys its own red blood cells. This leads to severe anemia and can cause life-threatening complications, including organ failure and blood clots. Key signs to watch for include extreme lethargy, pale or yellow gums, dark-coloured urine, and collapse. Diagnosis is confirmed through specific blood tests, including a slide agglutination test and a Coombs’ test. Treatment for IMHA in dogs is aggressive, focusing on powerful immunosuppressive drugs to stop the attack, alongside supportive care like blood transfusions. The prognosis is guarded, especially in the early stages, but with prompt and intensive veterinary care, many dogs can and do achieve remission. If you notice any signs, immediate veterinary intervention is critical.
Table of Contents
Understanding IMHA in Dogs: When the Body Attacks Itself
As a veterinarian, explaining IMHA in dogs to worried owners requires a careful balance of urgency and clarity. It’s a complex disease, but its core mechanism is dangerously simple: it’s a case of mistaken identity on a cellular level.
What is Immune-Mediated Hemolytic Anemia (IMHA)?
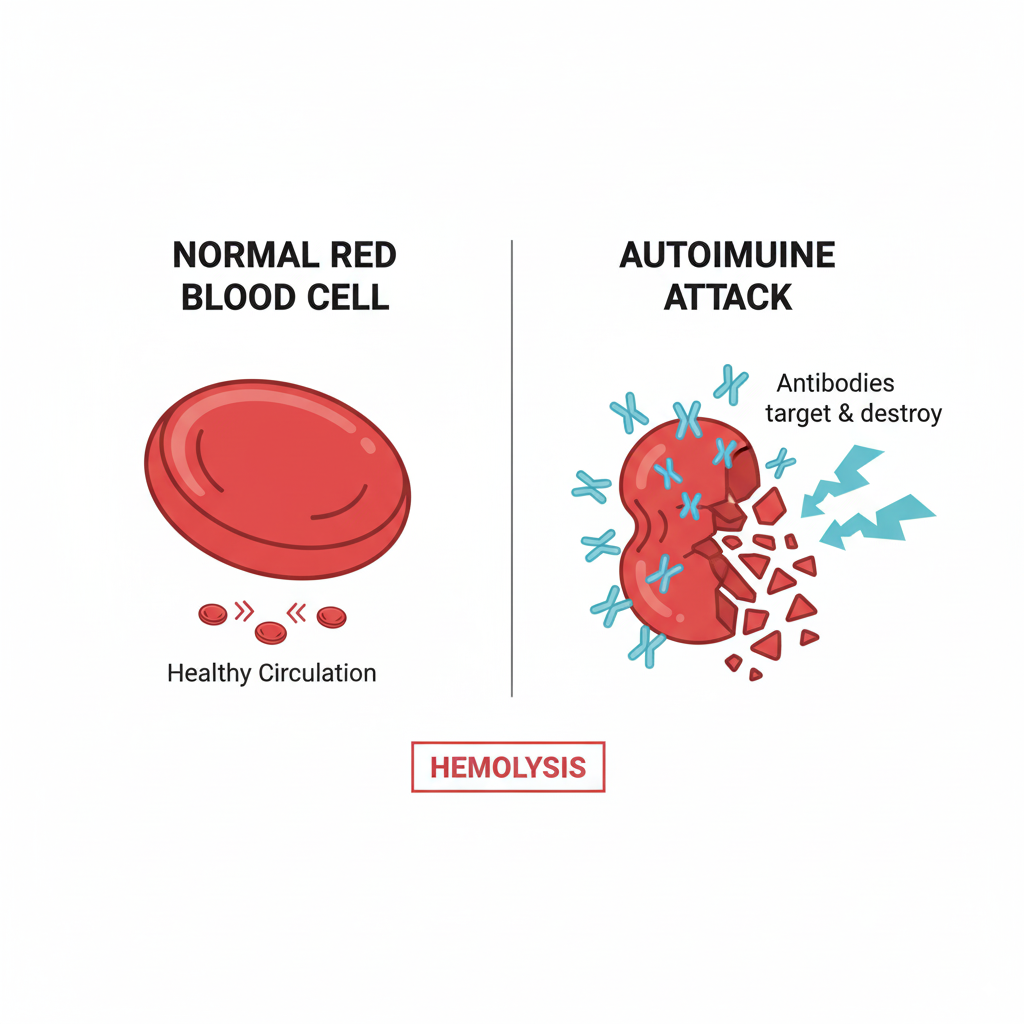
In the simplest terms, IMHA is an autoimmune disorder. Your dog’s immune system, which is designed to identify and destroy foreign invaders like bacteria and viruses, gets confused. It incorrectly flags its own red blood cells as a threat and produces antibodies that attach to them. These “tagged” red blood cells are then destroyed, a process called hemolysis.
When red blood cells are destroyed faster than the bone marrow can produce new ones, the result is anemia: a critical shortage of oxygen-carrying cells in the bloodstream. This oxygen deficit is what leads to the severe and sudden symptoms associated with the disease.
Primary vs. Secondary IMHA: What’s the Difference?
The veterinary community classifies IMHA in dogs into two main categories, and determining which type a dog has is crucial for treatment.
- Primary (or Idiopathic) IMHA: This is the most common form. “Idiopathic” is a medical term for “of unknown cause.” In these cases, the immune system dysfunction occurs spontaneously, without any identifiable underlying trigger. The diagnostic process is one of exclusion, meaning we run tests to ensure no other disease is kicking off the immune response.
- Secondary IMHA: This form is a reaction to an underlying issue that stimulates the immune system to attack the red blood cells. Potential triggers for secondary IMHA in dogs can include infections (like those from ticks), certain types of cancer, inflammatory conditions, or even reactions to some medications. Treatment for secondary IMHA requires addressing both the anemia and the root cause simultaneously.
7 Critical Signs of IMHA in Dogs You Shouldn’t Ignore
IMHA in dogs can progress with frightening speed. Seemingly mild signs can become a crisis in a matter of hours. If you observe any of the following, please treat it as an emergency.
- Extreme Lethargy: This is more than just being tired after a walk. It’s profound weakness, an unwillingness to move, or even the inability to stand up. This happens because the body is starved of oxygen.
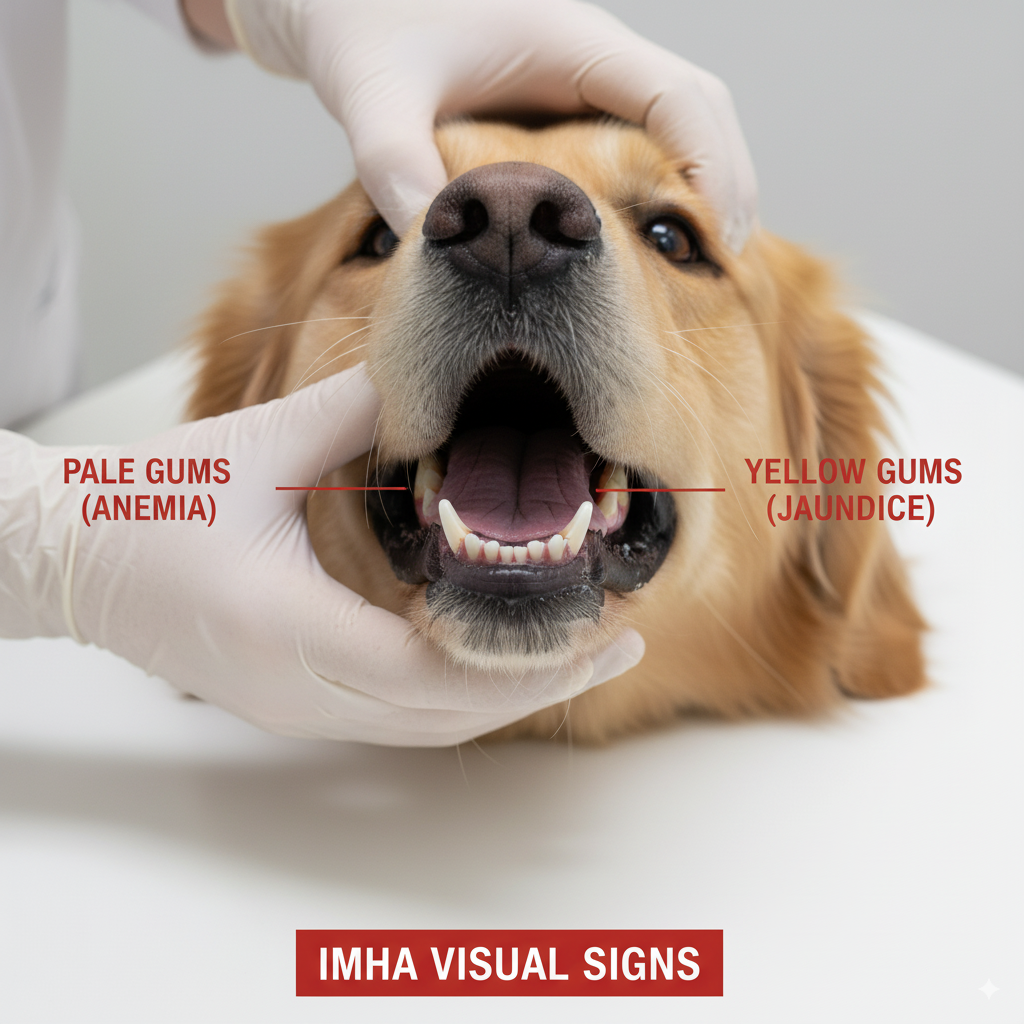
- Pale or Yellow Gums (Jaundice): Lift your dog’s lip. Gums that are white, pale pink, or yellow (jaundiced) are a hallmark of anemia and liver stress. The yellow tint comes from a substance called bilirubin, a byproduct of broken-down red blood cells that overwhelms the liver.
- Dark Red or Brown Urine: When red blood cells are destroyed in large numbers, the hemoglobin they contain is filtered through the kidneys and excreted in the urine, making it appear dark red, brown, or even black.
- Rapid or Laboured Breathing: The body tries to compensate for the lack of oxygen by breathing faster and harder. Your dog may be panting even while at rest.
- Collapse: An acute collapse is a sign of severe, life-threatening anemia and requires immediate veterinary attention.
- Vomiting or Diarrhea: The lack of oxygen can affect the gastrointestinal tract, leading to upset stomach and loss of appetite.
- Fever: A fever can be present as part of the body’s widespread inflammatory response.
Diagnosing IMHA: A Multi-Step Veterinary Process
In my veterinary experience, a suspected case of IMHA in dogs triggers a cascade of diagnostic tests designed to confirm the disease and rule out other causes quickly and accurately. The American College of Veterinary Internal Medicine (ACVIM) has established consensus guidelines to standardize this process.
READ MORE ABOUT HOW TO CHOSE A VETERINARIAN
Initial Blood Work: The First Clues
It all starts with blood work. A Complete Blood Count (CBC) gives us the most critical initial information. We look for:
- Severe Anemia: A very low red blood cell count (hematocrit) confirms the dog is anemic.
- Signs of Regeneration: We check if the bone marrow is trying to fight back by releasing immature red blood cells. The presence of these cells (reticulocytes) suggests a “regenerative anemia,” which is a classic sign of IMHA in dogs.
- Spherocytes: Under a microscope, we may see red blood cells that are smaller, darker, and more spherical than normal. These are cells that have been damaged by antibodies, and their presence is highly suggestive of IMHA.
Confirmatory Tests: Agglutination and Coombs’
While a CBC provides strong evidence, we need to confirm the immune-mediated component.
- Slide Agglutination Test: This is a rapid test we can perform in the clinic. A drop of blood is mixed with a drop of saline on a glass slide. If the red blood cells clump together (agglutinate), it’s a strong indicator that antibodies are coating them.
- Coombs’ Test (Direct Antiglobulin Test or DAT): This is the definitive test for IMHA in dogs. It is a laboratory test that directly detects the presence of antibodies or complement proteins attached to the surface of red blood cells, providing conclusive proof of an immune-mediated attack.
Once a diagnosis is confirmed, we often proceed with further diagnostics like X-rays and ultrasound to search for any underlying triggers of secondary IMHA.
Here is the second half of the draft.
Effective Treatment Protocols for IMHA in Dogs
Treating IMHA in dogs is an aggressive, multi-faceted process that requires intensive care, especially in the initial stages. The primary goals are to stop the immune system from destroying more red blood cells, support the body through the severe anemia, and prevent life-threatening complications. The approach is guided by detailed evidence-based consensus statements from the American College of Veterinary Internal Medicine (ACVIM).
The Core of Treatment: Immunosuppression
The cornerstone of treating IMHA in dogs is immunosuppression. We need to turn down the immune system’s overactive response as quickly as possible. This almost always starts with:
- Corticosteroids: High doses of corticosteroids (like prednisone) are the first line of defence. They are powerful, fast-acting drugs that suppress the immune response.
- Adjunctive Immunosuppressants: Because high-dose steroids can have significant side effects, and because they are not always enough on their own, a second immunosuppressive drug is often started at the same time. Options may include mycophenolate, cyclosporine, or azathioprine, which work in different ways to dial back the immune attack. The choice of drug depends on the individual case and veterinarian’s preference.
The goal is to eventually taper the patient down to the lowest effective dose of medication to maintain remission and minimize side effects. This tapering process can take many months.
Supportive Care: Blood Transfusions and Clot Prevention
While immunosuppressants work to solve the root problem, the patient needs immediate support to survive the anemia.
- Blood Transfusions: For dogs with severe, life-threatening anemia, blood transfusions are essential. A transfusion provides a fresh supply of red blood cells to carry oxygen to vital organs, buying precious time for the immunosuppressive drugs to take effect.
- Antithrombotic Medication: One of the most dangerous complications of IMHA in dogs is the formation of blood clots (thromboembolism). The widespread inflammation in the body creates a hypercoagulable state, meaning blood is more likely to clot. These clots can travel to the lungs, brain, or other organs with fatal consequences. Therefore, nearly all dogs treated for IMHA are placed on antithrombotic (anti-clotting) medications.

In very severe cases that are unresponsive to standard therapy, advanced techniques like immunoadsorption—a process that filters harmful antibodies from the blood—are being explored, though they remain experimental.
Your At-Home Care Checklist for a Dog with IMHA
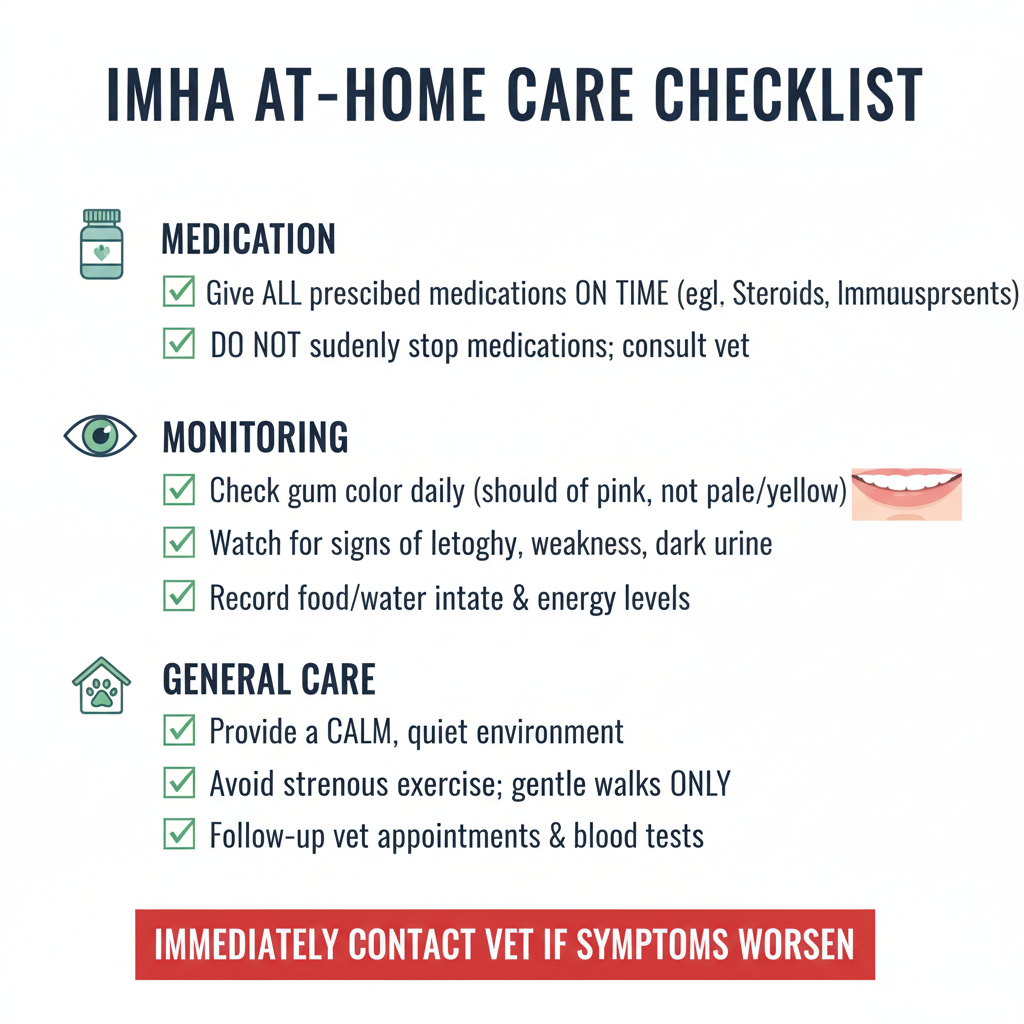
Bringing a dog home after they’ve been hospitalized for IMHA is a huge step, but the work isn’t over. Your diligence at home is critical for a successful recovery.
- Strict Medication Adherence: Give all medications exactly as prescribed. Do not alter doses or stop any drug without direct veterinary instruction. Use a pill organizer and set daily alarms.
- Monitor Gums Daily: Check your dog’s gum colour twice a day. Get a baseline of their “new normal” pink and watch for any return of paleness or a yellow tinge.
- Observe Energy Levels: Keep a simple daily log of your dog’s energy, appetite, and breathing rate. A sudden return to lethargy is a red flag.
- Create a Low-Stress Environment: Recovery requires rest. Limit strenuous activity, avoid dog parks or high-excitement situations, and provide a quiet, comfortable space.
- Watch for Relapse Signs: Be vigilant for any return of the initial symptoms: pale gums, weakness, or dark urine. Relapses are possible, and catching them early is crucial.
- Never Miss a Recheck: Follow-up blood work is essential to monitor your dog’s response to treatment and guide the medication tapering process.
The Cost of Treating IMHA in Dogs in Canada
Treating IMHA in dogs is financially demanding due to the need for intensive care, hospitalization, and long-term medication. Costs can vary significantly based on location and the severity of the case.
| Service / Item | Estimated Canadian Cost Range | Notes |
| Initial Diagnosis | $500 – $1,500 CAD | Includes emergency exam, comprehensive blood work, Coombs’ test, and imaging. |
| Hospitalization (per day) | $800 – $2,000+ CAD | Includes IV fluids, monitoring, and supportive medications. ICU care is at the higher end. |
| Blood Transfusion (per unit) | $700 – $1,200 CAD | Severely anemic dogs may require multiple transfusions. |
| Long-Term Medications | $100 – $400+ CAD per month | Cost depends on the size of the dog and the specific immunosuppressants used. |
| Follow-up Vet Visits & Blood Work | $200 – $500 CAD per visit | Frequent rechecks are needed, especially in the first few months. |
| Total Initial Cost (First Week) | $3,000 – $10,000+ CAD | This reflects the typical cost for a moderate to severe case requiring hospitalization. |
4 Key Prevention & Management Strategies for IMHA
While primary IMHA in dogs cannot be prevented, responsible management and awareness can improve long-term outcomes and help manage secondary IMHA.
- Consistent Parasite Prevention: Since tick-borne diseases can trigger secondary IMHA, year-round, vet-approved flea and tick prevention is a simple and effective protective measure.
- Judicious Vaccination: Work with your veterinarian to establish a vaccination schedule that is appropriate for your dog’s lifestyle and risk profile. Avoid over-vaccinating, as this can sometimes stimulate the immune system.
- Adhere to Tapering Schedules: For a dog in remission, the single most important factor for preventing relapse is following the medication tapering schedule precisely. Reducing doses too quickly can allow the immune attack to reignite.
- Immediate Action on Relapse: Know the signs of a relapse. A recent study from 2024 highlights that relapses are a recognized complication of the disease. At the first sign of returning symptoms, contact your veterinarian immediately. Early intervention is key.
Frequently Asked Questions About IMHA in Dogs
What is the survival rate for a dog with IMHA?
The prognosis for IMHA in dogs is guarded. Studies have shown mortality rates can be high, with some reports indicating about 50% of dogs may not survive the initial two weeks of treatment due to severe complications like blood clots. However, for dogs that stabilize and respond to treatment, the long-term prognosis improves significantly.
Can a dog fully recover from IMHA?
Yes, many dogs can go into remission, where the disease is controlled and they no longer require high doses of medication. While some dogs may eventually be weaned off all drugs, many require a low maintenance dose of an immunosuppressant for life to prevent relapse. A full “cure” is rare, and it is better to think of it as a manageable, chronic disease.
Are certain dog breeds more at risk for IMHA?
Yes, certain breeds appear to be genetically predisposed to developing IMHA in dogs. These include Cocker Spaniels, Poodles, Irish Setters, and Old English Sheepdogs. However, any dog of any breed can be affected.
Does IMHA in dogs cause pain?
The disease process itself—the destruction of red blood cells—is not typically considered painful. However, the consequences of severe anemia, such as oxygen deprivation to tissues, laboured breathing, and diagnostic or treatment procedures (like catheter placement), can cause significant discomfort and distress.
How We Researched This Article
To provide the most accurate and authoritative information on IMHA in dogs, our process is grounded in veterinary expertise and evidence-based medicine. This article was written by a licensed veterinarian and fact-checked against the 2019 ACVIM Consensus Statements on the diagnosis and treatment of IMHA, which are the gold standard for clinical practice. All claims are supported by hyperlinks to peer-reviewed research and trusted veterinary health institutions.
Conclusion
A diagnosis of IMHA in dogs is a challenging and often heart-wrenching journey. The path forward involves aggressive treatment, meticulous monitoring, and a deep partnership with your veterinary team. While the statistics can be daunting, advances in veterinary medicine and a better understanding of the disease are improving outcomes. Your commitment to their care—from the stress of the ICU to the quiet routine of at-home medication—is the most powerful tool in giving your loyal companion the best possible chance to lead a long and happy life.
References
- Swann, J.W., Garden, O.A., Fellman, C.L., Glanemann, B., Goggs, R., LeVine, D.N., Mackin, A.J., & Whitley, N.T. (2019). ACVIM consensus statement on the treatment of immune-mediated hemolytic anemia in dogs. Journal of Veterinary Internal Medicine, 33(3), 1141–1172. https://pubmed.ncbi.nlm.nih.gov/30847984/
- Garden, O.A., Fellman, C., Goggs, R., LeVine, D.N., Swann, J.W., & Szladovits, B. (2019). ACVIM consensus statement on the diagnosis of immune-mediated hemolytic anemia in dogs and cats. Journal of Veterinary Internal Medicine, 33(3), 1130–1140. https://pubmed.ncbi.nlm.nih.gov/30806491/
- Zhao, Q., Liu, J., Jiang, Y., Liu, H., Cui, N., & Liu, J. (2024). Investigation of risk factors for relapse in dogs with primary immune-mediated hemolytic anemia. Veterinary Research Communications, (online ahead of print). https://pubmed.ncbi.nlm.nih.gov/39235775/
- Haley, O., Woolcock, A.D., & Blais, M.C. (2020). Transcriptome analysis of whole blood in dogs with primary immune-mediated hemolytic anemia. Veterinary Immunology and Immunopathology, 229, 110123. https://pubmed.ncbi.nlm.nih.gov/33091028/
- Garden, O.A. (2011). Canine idiopathic immune-mediated haemolytic anaemia: a review of 50 years of research. The Veterinary Record, 169(20), 529. https://pubmed.ncbi.nlm.nih.gov/22029883/
- Ellermann, J., Tschirdewahn, J., Hofer-Schmitz, K., Mischke, R., & Tipold, A. (2021). Immunoadsorption as an adjunctive therapy in a dog with severe immune-mediated hemolytic anemia. Case Reports in Veterinary Medicine, 2021, 9977876. https://pubmed.ncbi.nlm.nih.gov/34033686/
- Carney, S.L., & Bright, L.A. (2016). Canine Autoimmune Hemolytic Anemia: Management Challenges in a Critical Case. Topics in Companion Animal Medicine, 31(3), 126-131. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6055891/




Pingback: 7 Important Facts on Steroid Use in Dogs