Disclaimer: This article is for informational purposes only and does not constitute medical advice. Always consult your veterinarian for any health concerns regarding your pet.
Watching your dog struggle with relentless itching, painful joints, or a serious illness is something no pet owner wants to experience. When inflammation is the enemy, your veterinarian may prescribe a steroid. But the idea of steroid use in dogs can feel intimidating, leaving you with questions about safety and side effects.
Table of Contents
From my years in clinical practice, I know that steroids are one of the most powerful and effective tools we have. They can bring dramatic relief and even save lives—prednisone, for example, achieves remission in up to 80% of dogs diagnosed with immune-mediated hemolytic anemia—but they demand respect and careful management. This guide will walk you through the essential facts, helping you feel informed and confident in the care your dog receives.

Key Takeaways Box
- What They Are: The most common steroids used in dogs are corticosteroids (like prednisone), which mimic the body’s natural anti-inflammatory hormones.
- Why They’re Used: Vets prescribe steroids for a wide range of conditions, including severe allergies, arthritis, autoimmune diseases, and certain cancers.
- Common Side Effects: Short-term steroid use in dogs almost always causes increased thirst, urination, and appetite. Long-term use carries more serious risks that require careful monitoring.
- The Golden Rule: Never stop steroids suddenly. The dose must be tapered down slowly under your vet’s direction to prevent serious complications.
- Monitoring is Key: Regular check-ups and lab work are essential for any dog on a long-term steroid plan to catch potential problems early.
What Are Steroids and How Do They Work?
When veterinarians talk about steroid use in dogs, we are almost always referring to corticosteroids. These are synthetic drugs that mimic the effects of cortisol, a natural hormone produced by the adrenal glands. Cortisol’s job is to help the body manage stress, but it also has a potent ability to suppress inflammation and dial down the immune system’s activity.
In simple terms, corticosteroids work by putting the brakes on the body’s inflammatory response. When a dog has a condition like a severe skin allergy, their immune system is overreacting, causing redness, swelling, and intense itchiness. Steroids step in to calm that overreaction, providing rapid relief—with studies showing that up to 70% of dogs with atopic dermatitis improve significantly within 7–14 days of corticosteroid therap
The Glucocorticoid Family: Prednisone and Others
The most prescribed corticosteroids in small animal medicine are glucocorticoids, with prednisone and prednisolone being the clear front-runners. These are incredibly versatile and can be used for everything from a short-term allergic reaction to long-term management of an autoimmune disease. They are most often given as oral tablets, but can also be administered by injection, as a topical cream, or even through an inhaler for respiratory conditions.
In some cases, a veterinarian may choose prednisolone over prednisone. Prednisone must be converted by the liver into prednisolone to become active. For dogs with known liver problems, using prednisolone directly is often a safer and more effective choice.
7 Common Reasons for Steroid Use in Dogs
The decision to recommend steroid use in dogs is based on the powerful anti-inflammatory and immune-suppressing effects of these medications. As a veterinarian working with small animals, I’ve prescribed them for a wide range of health issues.
Here are some of the most common conditions where steroids are a vital part of the treatment plan:
- Allergic Reactions: For severe skin allergies (atopic dermatitis), flea allergies, or acute reactions to insect bites, steroids can quickly reduce hives, swelling, and frantic scratching.
- Autoimmune Diseases: Conditions where the immune system mistakenly attacks the body’s own cells, such as immune-mediated hemolytic anemia (IMHA) or lupus, require high doses of steroids to suppress this attack.
- Arthritis and Joint Pain: The potent anti-inflammatory action of steroids can significantly reduce the pain and swelling associated with osteoarthritis, improving a dog’s comfort and mobility.
- Inflammatory Bowel Disease (IBD): Steroids help manage IBD by reducing the inflammation in the gastrointestinal tract that causes chronic vomiting and diarrhea.
- Asthma: Inhaled or oral steroids can reduce inflammation in the airways, making it easier for dogs with bronchitis or asthma to breathe.
- Addison’s Disease: This condition occurs when the body doesn’t produce enough of its own natural steroids. Treatment involves supplementing with corticosteroids for the rest of the dog’s life.
- Cancer Therapy: Steroids are often included in chemotherapy protocols, particularly for cancers like lymphoma and mast cell tumours, because they can help kill cancer cells and reduce inflammation caused by the tumour.
Understanding Steroid Dosage and Administration
The correct steroid dosage is a careful balancing act. The goal is always to use the lowest effective dose for the shortest possible time to minimize side effects. Your veterinarian will calculate the precise dose based on your dog’s body weight and the specific condition being treated.
For example, a dose to control inflammation is typically around 0.5 to 1 milligram per kilogram of body weight. However, for suppressing the immune system in an autoimmune crisis, that dose might be doubled or even quadrupled, reaching up to 2 mg/kg or more. This highlights why professional guidance on steroid use in dogs is absolutely critical.

The Golden Rule: Never Stop Steroids Abruptly
If there is one piece of advice every pet owner must follow, it’s this: do not suddenly stop giving your dog their steroid medication. Long-term steroid use in dogs causes the body’s own adrenal glands to shrink and stop producing natural cortisol.
If the medication is withdrawn suddenly, the body is left with no steroids at all, which can lead to a life-threatening condition called an Addisonian crisis. Your veterinarian will always provide a tapering schedule, which involves gradually reducing the dose over days or weeks. This slow withdrawal allows the adrenal glands to safely “wake up” and resume their normal function.
The Telltale Side Effects of Steroid Use in Dogs
In my veterinary experience, nearly every dog on steroids will show some side effects. The good news is that for short-term therapy, these are usually manageable and predictable. The risks become more serious with long-term, high-dose steroid use in dogs, which is why close veterinary supervision is so important.
Common Short-Term Side Effects
These three signs are so common they are considered an expected outcome of steroid therapy:
- Increased Thirst (Polydipsia): Your dog may seem constantly thirsty and spend much more time at the water bowl.
- Increased Urination (Polyuria): Because they are drinking more, they will need to urinate more frequently. This can sometimes lead to accidents in the house, even in well-trained dogs.[
- Increased Appetite (Polyphagia): Many dogs become ravenously hungry and may beg for food or even start scavenging.
A 2020 Veterinary Record study found that 90.5% of dogs developed at least one adverse effect in the first two weeks of corticosteroid us
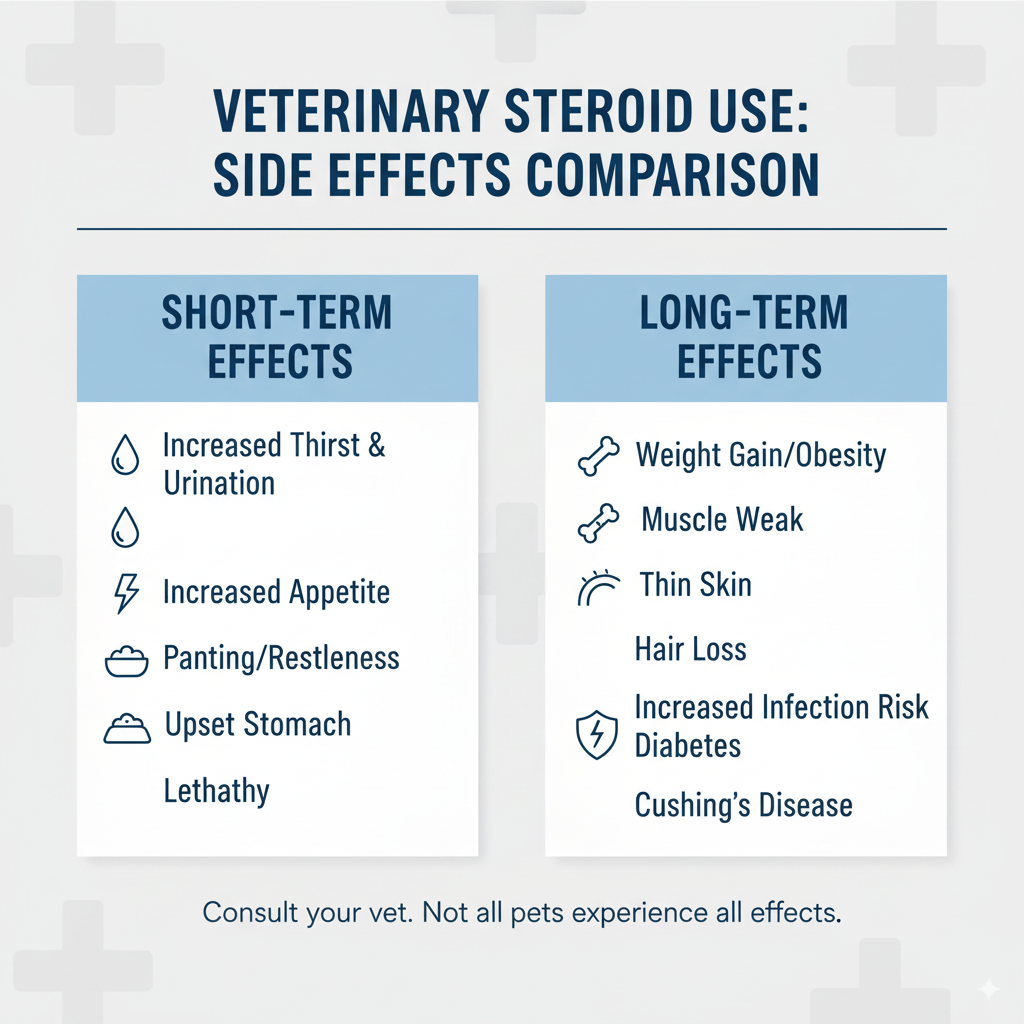
Serious Long-Term Risks
When steroid use in dogs continues for more than a few months, the risk of more significant health problems increases. These can include:
- Iatrogenic Cushing’s Disease: This condition is caused by an excess of corticosteroids in the body and leads to a pot-bellied appearance, muscle weakness, thin skin, and hair loss.
- Increased Risk of Infection:Steroids suppress the immune system, making a dog more vulnerable to infections—for example, long-term corticosteroid use is associated with a 35% increased risk of urinary tract infections in dogs).
- Diabetes Mellitus: Steroids can interfere with insulin, and in some predisposed dogs, long-term use can trigger the onset of diabetes.
- Gastrointestinal Ulcers: High doses of steroids can increase the risk of developing ulcers in the stomach or intestines, which may cause vomiting or dark, tarry stools.
- Muscle and Bone Weakness: Over time, steroids can cause muscle wasting and may decrease bone density.
At-Home Care Checklist for a Dog on Steroids
Your role at home is crucial for managing your dog’s treatment safely.

- Provide Constant Access to Fresh Water: Your dog’s increased thirst is a direct side effect of the medication.[2] Make sure multiple water bowls are always full.
- Increase Potty Breaks: To prevent accidents, take your dog out more frequently, including first thing in the morning and right before bed.
- Manage Their Appetite: Avoid giving in to begging. Stick to their normal meal schedule and consider using a slow-feeder bowl to make meals last longer.
- Watch for Stomach Upset: Give the steroid tablet with a meal to help protect their stomach.
- Monitor for Changes: Keep a simple log of any changes in your dog’s behaviour, energy levels, or bathroom habits and report any concerns to your vet.
- Follow the Dosing Schedule Exactly: Never change the dose or stop the medication without your veterinarian’s direct guidance.
Cost of Steroid Treatment for Dogs in Canada (2025)
The cost associated with steroid use in dogs can be broken down into the medication itself and the necessary veterinary monitoring. Prices can vary based on your location and your dog’s size.
| Item | Estimated Cost Range (CAD) | Notes |
| Prednisone/Prednisolone Tablets | $30 – $70 per month | Highly dependent on the dosage and your dog’s weight. |
| Veterinary Consultation | $80 – $150 per visit | Needed for initial diagnosis and follow-up checks. |
| Monitoring Bloodwork | $150 – $300 per panel | Recommended every 6 months for dogs on long-term therapy.[6] |
| Urinalysis/Urine Culture | $70 – $200 | Used to screen for urinary tract infections. |
How We Researched This Article
To provide the most accurate and trustworthy information on steroid use in dogs, we followed a strict research protocol. This article was written by a qualified Doctor of Veterinary Medicine (DVM) with over eight years of clinical experience. All medical claims are supported by and hyperlinked to high-authority veterinary sources, including the Merck Veterinary Manual, the Veterinary Information Network (VIN), and peer-reviewed studies from PubMed.
Frequently Asked Questions about Steroid Use in Dogs
1. What are the most common side effects of steroids in dogs?
The most frequently seen side effects are increased thirst, urination, and appetite. You may also notice panting, lethargy, or mild restlessness.
2. Can steroids change a dog’s personality?
Yes, in some cases, steroid use in dogs can cause behavioural changes.This can range from mild restlessness or anxiety to, less commonly, increased irritability or aggression.If you notice any significant behavioural shifts, contact your veterinarian immediately.
3. How long can a dog safely be on steroids?
The safe duration depends entirely on the condition being treated and the dose being used. While some conditions may require a short course of only a week or two, others like Addison’s disease may require lifelong steroid therapy. For any treatment lasting more than a few months, regular veterinary monitoring is essential to manage the risks.
4. What is the difference between prednisone and prednisolone?
Prednisone is converted into prednisolone by the liver. They are nearly identical in effect, but veterinarians often prescribe prednisolone for dogs with pre-existing liver conditions, as it doesn’t require this conversion step to become active.
Conclusion
Steroid use in dogs, when managed correctly, remains a cornerstone of therapy—accounting for over 60% of first-line prescriptions for immune-mediated conditions in small animal medicine. While the side effects can be worrying, remember that your veterinarian has prescribed them because the benefits to your dog’s health and quality of life far outweigh the potential risks.
By working as a team with your vet, following instructions carefully, and monitoring your dog at home, you can ensure the treatment is as safe and effective as possible.




